The holiday season is upon us and it promises to be one like no other. Our colleagues in Massachusetts are having to “curtail” inpatient elective surgery and many others of us are or have been under similar restrictions. None of this is surprising, as epidemiologists consistently predicted a “second wave” in late fall. This increase in COVID-19 cases is different from the one that occurred in the spring.
First, we have a better understanding of COVID’s pathophysiology now, and our ability to treat patients is vastly improved. The two available antibody infusions have shown promise in mitigating COVID-19’s effects and decreasing hospitalizations. Furthermore, our ability to test and trace patients is much better than it was in the spring. Most importantly, there is a viable vaccine that will soon be widely available.
These factors will lessen the effects of this second wave on our patients and profession. Additionally, because of the efforts of AAOS and its volunteers, we have a more cogent, evidenced-based algorithm for the handling of elective orthopaedic surgery in the face of COVID-19. This will obviate the wholesale cessation of our surgery and avoid a repeat of what transpired in the spring. We should be grateful for all of the above.
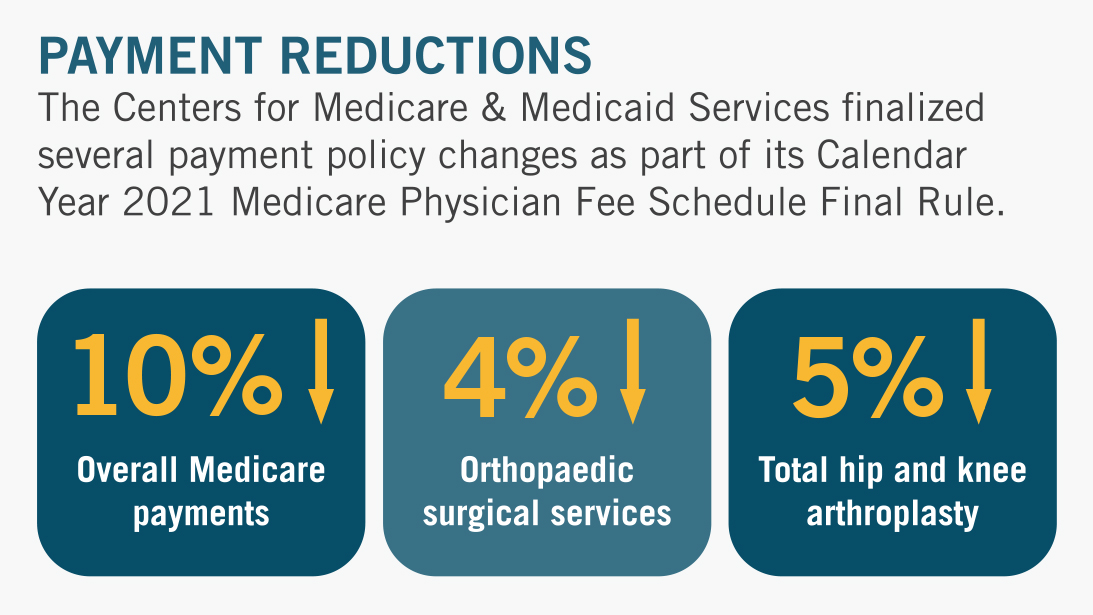
Meanwhile, the Centers for Medicare & Medicaid Services (CMS) recently finalized the 2021 Medicare Physician Fee Schedule (MPFS) four months after the changes were proposed. The document is over 1,000 pages long, but the following are the salient points (see AAOS summary):
- CMS is increasing the work Relative Value Units (RVU) for office/outpatient evaluation and management (E/M) codes, including codes 99202-99215.
- CMS is eliminating code 99201.
- CMS is decreasing the 2021 conversion factor by 10.2 percent ($36.09 for 2020, down to $32.41 for 2021), citing a statutory mandate for budget neutrality resulting from changes in the E/M work RVUs.
- CMS is finalizing its proposal to decrease the work RVU of codes 27130 and 27447 (total hip and knee replacements) from 20.72 to 19.60, a 5% reduction.
- CMS is asking for comment on how to include pre-optimization time (pre-service work/activities ancillary to surgical outcome improvement) in the future. This would reimburse orthopaedic surgeons for time spent optimizing patients in the pre-operative period and offset the decreased total joint work RVUs.
- CMS finalized a policy to adopt the new coding framework. Under this new CPT coding framework, history and exam will no longer be used to select the level of code for office/outpatient E/M visit codes. Instead, levels of decision-making and time spent will be used.
- CMS is finalizing its proposal to adjust E/M visit codes without applying the revisions to 10- and 90-day global surgical codes.
Although not surprised by the 2021 final rule, the AAOS is deeply disappointed by the temerity of the Federal Government in decreasing our reimbursement in the midst of the COVID-19 pandemic. Furthermore, the legally mandated budget neutrality provisions mean that any increase in reimbursement for office/outpatient E/M codes results in a decrease in reimbursement for other codes or payments. This zero-sum game divides the “House of Medicine,” pitting cognitive specialists (i.e., neurologists and internists) against surgeons. When the proposed rules came out this August, our Office of Government Relations (OGR) organized multiple call-in meetings with policymakers within CMS, HHS and OMB. We combined and coordinated these efforts with the American Association of Hip and Knee Surgeons (AAHKS) and several non-orthopaedic surgical specialties. We spoke, they listened, and little was changed. Again, we anticipated that this might happen so we, in parallel, were working on plans to prevent these cuts from becoming law.
Medicare Payment Policy Changes for 2021
An interactive infographic timelining CMS policy changes with AAOS advocacy.
The U.S. House of Representatives introduced the Holding Providers Harmless from Medicare Cuts During COVID-19 Act of 2020 (H.R. 8702). This vital legislation would hold negatively impacted healthcare professionals harmless from the cuts for both 2021/2022. The OGR formed and is leading a coalition of musculoskeletal organizations that are jointly offering their support for this piece of legislation. The bill’s original group of seven sponsors, which included physician U.S. Representatives Ami Bera, MD; Larry Bucshon, MD; Phil Roe, MD; and Raul Ruiz, MD, and non-physician U.S. Representatives Brendan Boyle, George Holding and Abby Finkenauer, has now grown to over 90 Representatives.
The Senate also introduced a companion bill—S. 5007—late last week, demonstrating the groundswell of support for a solution to avert the cuts across both parties and chambers. There are two potential opportunities remaining this year for a policy solution to progress, with Congress having to pass a spending bill, as well as renew expiring healthcare extenders. Congress could also include a solution in a COVID-19 relief package, but negotiations have stalled on numerous occasions due to disagreements around key provisions by both Democrats and Republicans.
This legislation is supported by nearly 400 medical organizations, including the American Medical Association (AMA) and the American College of Surgeons (ACS). Congressional sources credit the high volume of outreach they have received from the specialty healthcare community, citing the grassroots messages that have been pouring into Capitol Hill offices requesting congressional intervention. With limited days remaining for legislative activity, AAOS will continue to strongly advocate on behalf of orthopaedic surgeons on this issue and work to preserve the value of specialty care.
The OGR is fully mobilized and completely focused on getting H.R. 8702/S. 5007 to become law. We are working with AAHKS and mounting a grassroots effort through the Board of Specialty Societies (BOS) and the Board of Councilors (BOC). We ask that you lend your support to this effort by logging on to the AAOS Advocacy Action Center and contacting your federal representatives on this issue. This is our best chance at heading off these cuts and maintaining our patients’ access to care.
Lastly, I would be remiss if I did not mention that Congress announced a deal late Friday night on surprise medical billing (see AAOS summary). Your Academy has been heavily engaged on this issue since 2018, working with our allies in Congress and other coalition members to both protect patients from unexpected bills while ensuring that physician practices have access to a process for negotiating payment for out-of-network care. While the solution being presented isn’t perfect, we can see how much it has been heavily influenced by the principles we’ve stood for. We will continue to advocate for improving the independent dispute resolution process and all the bill’s provisions at every opportunity, including during crucial federal rulemaking following the expected passage of the legislation.
Thanks, and have a wonderful holiday season.
Joseph A. Bosco, III, MD, FAAOS
AAOS President