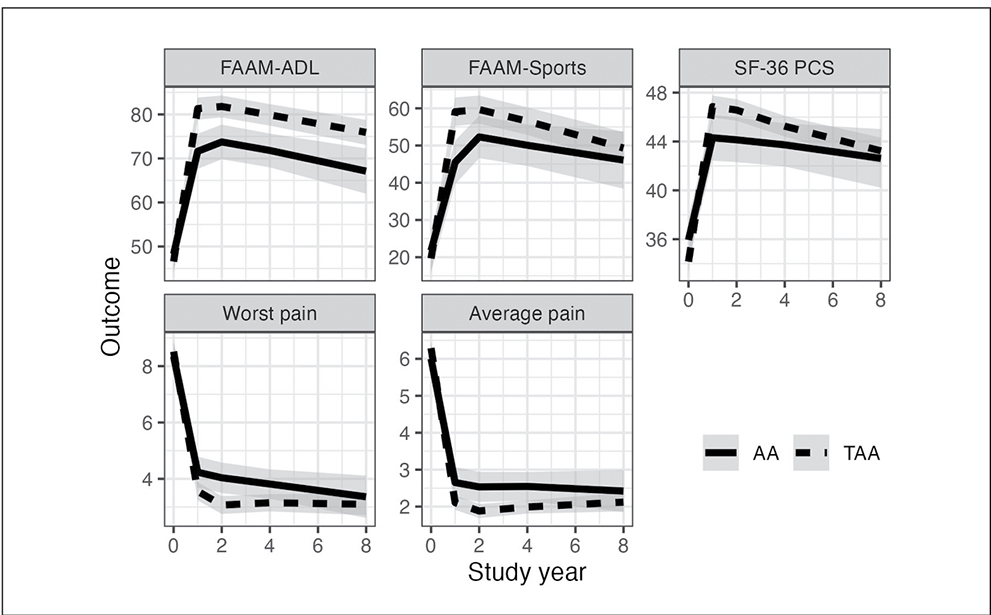
FAAM, Foot and Ankle Ability Measure; ADL, activities of daily living; SF-36 PCS, 36-Item Short Form Survey physical component summary
A new study being presented at the AAOS 2025 Annual Meeting reported that ankle arthrodesis (AA) and total ankle arthroplasty (TAA) are both effective for end-stage ankle arthritis (ESAA) up to 8 years. Both treatments provided pain relief and improved patient-reported functional outcomes in this long-term follow-up analysis.
ESAA is a debilitating and painful condition with major effects on function and quality of life. When patients fail conservative management, such as anti-inflammatory medications, corticosteroid injections, bracing, or physical therapy, they may be offered ankle fusion or joint replacement.
Researchers conducted a study comparing results between the two procedures at 2, 4, and 8 years postoperatively because they were “convinced of the clinical equipoise of the two treatments,” said presenting author Bruce J. Sangeorzan, MD, FAAOS, professor of orthopaedics and sports medicine at the University of Washington and director of the VA Center of Excellence in Limb Loss Prevention and Prosthetic Engineering in Seattle. “At the time we began this study, many patients were reluctant to consider ankle replacement, as most orthopaedic surgeons believed it was not a safe alternative. Further, ankle fusion was a very successful operation. Unlike the hip or knee, ankle fusion did not interfere much with activities of daily living. So there was a clear knowledge gap in the physician education and patient education arena for the appropriate use of ankle replacement.”
The study enrolled patients who were seeking surgery for ESAA at six sites from May 2012 to May 2015. To be included, patients had to be eligible for both procedures. Exclusion criteria included systemic diseases such as inflammatory arthritis or other health conditions that affected gait. Before surgery and at 12-month intervals, the patients completed several measures: Foot and Ankle Ability Measure scales for activities of daily living and sports, 36-Item Short Form Survey (SF-36) for physical and mental health component summaries, a numeric rating scale for pain, and patient satisfaction questions.
“We set out to find patient-reported outcome measures that were sensitive to the clinical problems patients identified as important. And we added an objective measure of activity particularly useful when managing explanations of outliers. Additionally, we used individual change scores for each subject rather than pool scores so that we could be certain that our loss to follow-up could be managed. Other studies used group patient-reported outcomes,” Dr. Sangeorzan explained.
Participating surgeons for both procedures were board-certified orthopaedic surgeons with foot and ankle fellowship training. All surgeons had demonstrated expertise in AA and TAA.
The study included 522 patients (419 TAA and 103 AA). Follow-up scores were available in 426 (82 percent) at 4 years, 346 (67 percent) at 6 years, and 269 (52 percent) at 8 years. Analysis of 8-year data revealed that both groups maintained strong improvement in all outcomes compared with pre-operative scores (Fig. 1). There was a slightly better trajectory of results for activity and patient-reported outcomes in the arthroplasty group at 2 years, 4 years, and 8 years. Risk of adverse events was similar between groups.
“Historically, arthroplasty is viewed as a less durable treatment option than arthrodesis. Some would expect the arthroplasty results to decay over time and become less successful than the arthrodesis group. This did not happen,” Dr. Sangeorzan noted. “My personal bias at the beginning of this study … was to reserve arthroplasty for patients over 65 years or patients who had no function in their triple joints or had bilateral disease. Over the 20 years since we began studying this problem, I’ve personally felt confident in using less restrictive application of arthroplasty, and I think other surgeons can as well.”
Poster P053 will be on display during Foot and Ankle Poster Session 1, Monday and Tuesday in OrthoLive.
Dr. Sangeorzan’s coauthors of “Ankle Function Is Sustained between 4 and 8 Years in a Long-Term Prospective Cohort Study of Ankle Arthroplasty versus Arthrodesis” are Daniel Norvell, PT; William R. Ledoux, PhD; J. Chris Coetzee, MD, FAAOS; James Davitt, MD, FAAOS; John G. Anderson, MD, FAAOS; Michael E. Brage, MD, FAAOS; Donald R. Bohay, MD, FAAOS, FACS; and Jane Shofer, MS.
Keightley Amen, BA, ELS, is a freelance writer for AAOS Now.