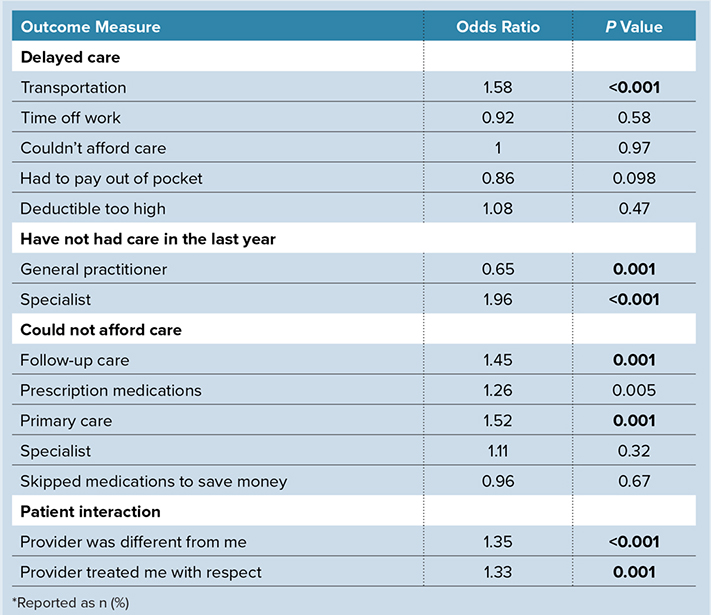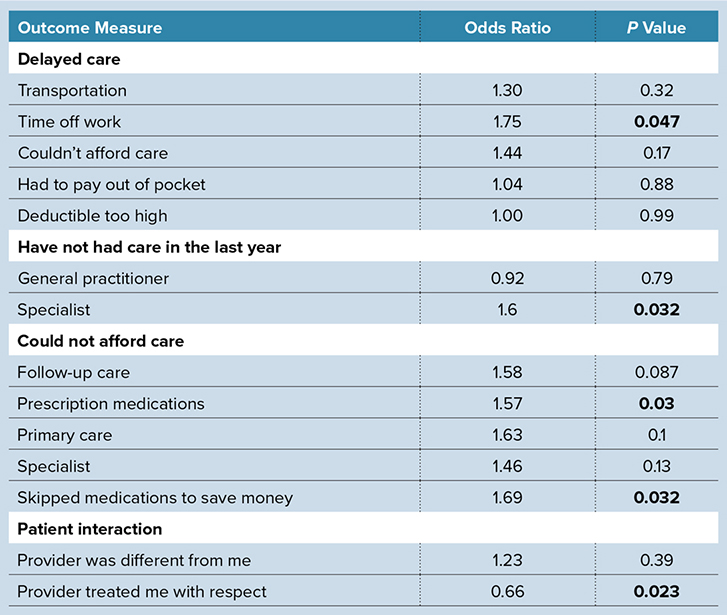
Bold indicates statistical significance (P <0.05).
Early diagnosis and treatment for osteoarthritis (OA) can improve symptoms, slow disease progression, and delay the need for joint replacement. Recent research presented at the AAOS 2025 Annual Meeting revealed specific barriers to OA care for Hispanic and Black patients, highlighting the need for targeted interventions. Hispanic patients were more likely to delay care due to challenges related to taking time off work, inability to afford prescription medications, and lack of access to specialists. Black patients faced obstacles including transportation difficulties, affordability of follow-up care and medications, and limited access to specialists.
“This research was particularly important as OA significantly affects the quality of life of millions of Americans, particularly in racial and ethnic minority groups who face pronounced barriers to care. Despite prior studies demonstrating disparities in OA progression and treatment utilization, few studies have explored the specific reasons preventing minority patients from accessing timely care,” said study coauthor Alex Holle, BS, a medical student at the Mayo Clinic Alix School of Medicine, who spoke with AAOS Now about the study.
Mr. Holle and colleagues used data from the Healthcare Access and Utilization Survey, part of the All of Us Research Program, to identify barriers to care for Hispanic and Black adults with hip, knee, or shoulder OA (Tables 1 and 2). They categorized patients into three groups based on self-reported race and ethnicity: Hispanic, Black, and non-Hispanic white. They also compared demographic variables such as age, gender, income, insurance status, employment status, and education level.
As compared with non-Hispanic White patients, Hispanic patients:
- received care for OA at a significantly younger age
- were significantly less likely to be insured or have a college degree
- were significantly more likely to delay care due to difficulties taking time off work
- were less likely to receive specialty care
- were more likely to be unable to afford prescription medications and were more likely to skip medications to save money
- were more likely to report that a healthcare professional had not treated them with respect
The researchers suggested that social determinants of health (SDOH), such as working more physically demanding jobs and having less access to preventive care to manage milder symptoms, could be factors in this population’s more severe disease and need for earlier care.
In addition, the study found that Black patients:
- were significantly more likely to experience delays in care due to transportation issues
- were less likely to have received care from general practitioners but more likely to have received care from specialists
- were more likely to be unable to afford follow-up care or prescription medications
- were more likely to delay or avoid care due to racial differences with healthcare professionals
The authors highlighted the potential role of structural systems of segregation and mistrust in the healthcare system in creating these barriers to care. They hypothesized that Black patients may be more likely to see specialists because they are unable or unwilling to seek medical attention until OA has progressed.
“This work emphasizes the urgency of addressing racial and ethnic disparities in OA care and highlights actionable factors that can drive meaningful change,” Mr. Holle said. “The findings represent real barriers that patients face every day, which can lead to delayed care, poorer outcomes, and greater health inequities. Addressing these disparities requires commitment at every level—providers, healthcare systems, policymakers, and communities.”
The researchers plan to explore these barriers at their own institution and identify strategies to address them, such as offering flexible scheduling and telehealth services, advocating for financial assistance programs to cover medications and follow-up care, and addressing interpersonal barriers through cultural competence training and a more diverse healthcare workforce.
Mr. Holle’s coauthors of “Unequal Access: Racial and Ethnic Disparities in Access to Healthcare for Patients with Osteoarthritis” are Camryn Sumwalt Payne, BA; Paul Ryan Van Schuyver, MD; and Joshua Bingham, MD, FAAOS.
Keightley Amen, BA, ELS, is a freelance writer for AAOS Now.