Anterior lumbar interbody fusion (ALIF) effectively restores L4–S1 lordosis in patients with severe sagittal deformity, according to the results of a study from the International Spine Study Group, presented during the AAOS 2024 Annual Meeting.
According to presenting author Alan H. Daniels, MD, FAAOS, chief of the Division of Spine Surgery at Brown University in Rhode Island, “Despite robust data describing the importance of spinal alignment and the well-known benefits of spinal deformity correction, there is still a lack of understanding regarding which techniques are best for the treatment of severe spinal malalignment.” Thus, his team sought to conduct a comparative study of pedicle subtraction osteotomy (PSO) versus ALIF versus transforaminal lumbar interbody fusion (TLIF) or other surgical techniques for restoration of optimal spinal shape from L4–S1.
The study included 98 patients with severe adult spinal deformity. Patients had preoperative pelvic incidence minus lumbar lordosis (PI-LL) of >20 degrees and L4–S1 lordosis of <30 degrees. full-body radiographs and patient-reported outcome measures were collected at baseline and at 6 weeks postoperatively. the treatment groups were split up as follows:
- 26 patients underwent ALIF (one or two ALIFs at L4–S1).
- 18 patients underwent PSO (at L4 or L5).
- 54 patients underwent “other” surgeries (TLIF or ALIF/lateral lumbar interbody fusion/osteotomy at L3 or more cranial levels).
The primary outcomes were postoperative radiographic alignment compared with baseline and 90-day complications.
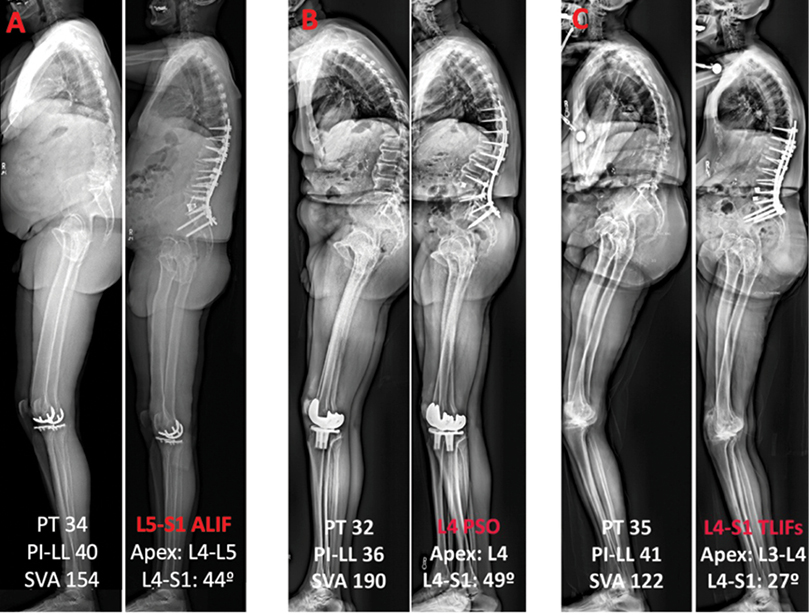
Fig. 1 shows pre- and postoperative radiographs of the spinal correction across ALIF, PSO, and TLIF. At the 6-week postoperative follow-up, L4–S1 correction was largest in the ALIF group (21 degrees) and PSO group (27 degrees) compared with the “other” treatment group (8 degrees; P <0.05). pelvic tilt correction was highest in the alif group (11 degrees) compared with pso and the other techniques (9 degrees and 7 degrees, respectively;>P <0.05). the alif and pso groups had greater pi-ll correction compared with other techniques (34 degrees and 32 degrees versus 26 degrees, respectively;>P <0.05). the apex of lumbar lordosis migrated caudally by 0.6 of a level in the alif group at 6 weeks, between l4 and l5 to around l4 (>P <0.05), but it did not change in the other groups.
Rates of intraoperative blood loss were highest in the PSO group (P <0.05), along with higher rates of postoperative sensory deficits (25 percent in the pso group versus 7 percent in the alif group and 4 percent in the “other” group;>P <0.05) and motor deficits (38 percent versus 11 percent and 9 percent, respectively;>P <0.05). overall, dr. daniels noted, “the patient outcomes were surprisingly good in this complex cohort of patients, likely due to the experience of the international spine study group surgeons, who have a tremendous amount of experience correcting the most severely misaligned spines.”
Based on these findings, he concluded, “ALIF can restore L4–S1 sagittal alignment as powerfully as PSO, with fewer intraoperative and in-hospital complications. When feasible, ALIF is a suitable alternative to PSO and likely superior to TLIF for correcting L4–S1 lordosis among patients with severe sagittal malalignment.” Although all the techniques analyzed were effective for correcting deformity, Dr. Daniels noted that ALIF in particular “may be most powerful for restoring a physiologic lordotic apex.”
He acknowledged several limitations, included the small sample and the experience of the surgeons, meaning that the results “may not be generalizable to surgeons with little experience correcting severe spinal deformity.” Looking ahead, Dr. Daniels stated that further research is needed for continued monitoring of long-term outcomes in this cohort and analyses of larger patient populations. He added, “Investigation of newer techniques will be needed to further our knowledge regarding lordosis restoration in severely misaligned patients.”
Dr. Daniels’ coauthors of “Restoring L4-S1 Lordosis Shape in Severe Sagittal Deformity: Impact of Correction Techniques on Alignment and Complication Profile” are Bassel Diebo, MD; Renaud Lafage; Kevin DiSilvestro, MD; Mariah Balmaceno-Criss; Daniel James Alsoof, MD; D. Kojo Hamilton, MD; Robert Kenneth Eastlack, MD, FAAOS; Richard G. Fessler, MD, PhD; Jeffrey Gum, MD, FAAOS; Munish C. Gupta, MD, MBA, FAAOS; Richard A. Hostin, MD, FAAOS; Khaled M. Kebaish, MD, FAAOS; Breton G. Line; Pierce Dalton Nunley, MD; Gregory Michael Mundis, MD; Peter Gust Passias, MD, FAAOS; Justin K. Scheer, MD; Alexandra Soroceanu, MD; Eric O. Klineberg, MD, FAAOS; Christopher Ames, MD; Robert Shay Bess, MD; Lawrence G. Lenke, MD; Frank J. Schwab, MD; Virginie Lafage, PhD; Christopher I. Shaffrey, MD, FAAOS; and Douglas C. Burton, MD, FAAOS.
Rebecca Araujo is the managing editor of AAOS Now. She can be reached at raraujo@aaos.org.