When utilizing intramedullary headless screws (IMHS) for fixation of metacarpal fractures, screw size may be related to incidence of radiographic displacement, according to results of an ePoster presented at the AAOS 2024 Annual Meeting.
“Intramedullary screw fixation avoids many of the complications associated with other forms of treatment of metacarpal fractures, including Kirschner wire [K-wire] or dorsal plating, as it is performed through a minimally invasive approach and affords sufficient stability for early range of motion (ROM),” study co-authors Gaurav Luther, MD, and Andrew Allen, MD, both of WakeMed Hospitals and University of North Carolina, told AAOS Now. “However, when placing an intramedullary screw, the surgeon currently has limited guidance in choosing the appropriate diameter. While a larger screw seems optimal for stability, larger screws also create a larger defect in the metacarpal head and have the potential for causing degenerative changes.”
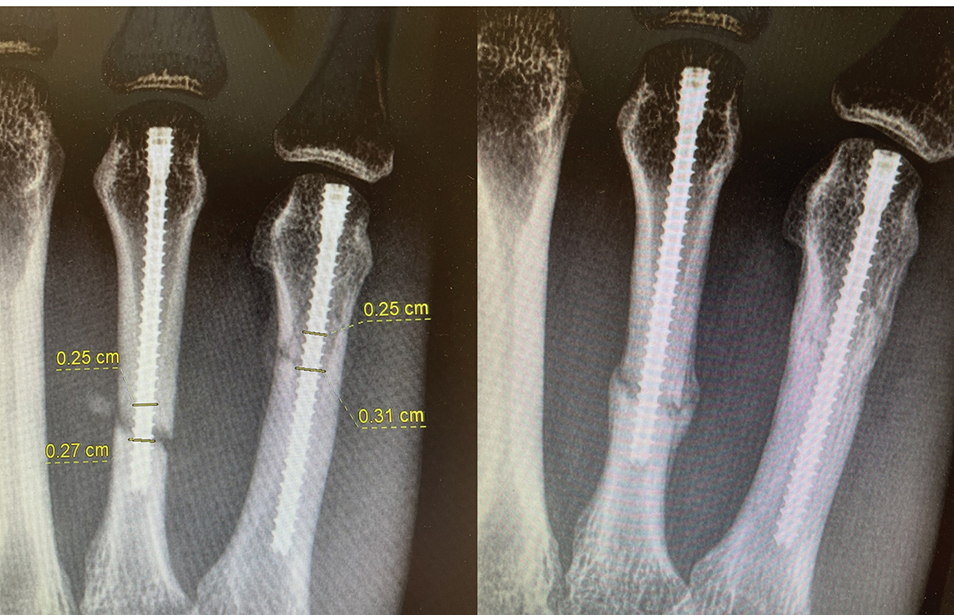
The investigators sought to evaluate the influence of screw diameter and the ratio of canal fill on clinical and radiographic outcomes. They retrospectively analyzed 52 patients with metacarpal fractures treated by a single surgeon between 2017 and 2022. Patients with open fractures, inadequate follow-up, and alternative treatments besides IMHS were not included. The analyzed procedure was retrograde IMHS through an ulnar sagittal band split. Patients were not immobilized postoperatively and initiated early ROM on postoperative day 2. Intraoperative radiographs were utilized to measure the ratio of screw diameter to metacarpal isthmus diameter at the fracture site.
The follow-up period was 6 months. Assessments included radiographic displacement; ROM; the Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) questionnaire; and patient satisfaction. The authors defined displacement on postoperative radiograph as angulation >10 degrees or displacement >2 mm.
“All 52 patients with 58 fractures included in our study had excellent clinical results,” Dr. Allen said. “There were seven cases of radiographic displacement following intramedullary screw fixation. Six of these cases occurred in the small finger metacarpal where the canal diameter is the largest. All cases of displacement were in oblique fracture patterns with 2.5 mm screws.” The average time to union was 6 weeks.
Regarding clinical outcomes, mean grip strength was 95 percent (range, 84–104 percent) relative to the contralateral side, and the average total active motion was 248 degrees (range, 240–260 degrees). The mean QuickDASH score was 2.1 (range, 0–9.1). No patients experienced extensor lag, and no revision surgeries were required.
There were no cases of radiographic displacement observed with 3.0 mm screws or when the screw diameter was >75 percent of the canal diameter. Notably, even in cases of radiographic displacement, clinical outcomes (i.e., satisfaction, QuickDASH scores, grip strength, ROM) were not negatively affected compared to cases without radiographic displacement.
“It was interesting that in patients with displaced fractures, we still observed excellent clinical outcomes,” Dr. Allen commented. “The radiographic data did not mirror patients’ clinical data. It was also surprising how uniform the characteristics were among the cases of fracture displacement.”
The main takeaway, according to Dr. Luther, is that surgeons may be able to “prevent radiographic displacement with larger screw diameters, particularly when the screw diameter is greater than 75 percent of the canal diameter. However, preventing radiographic displacement may not be of utmost importance, as patients with displacement still had excellent clinical outcomes.” He added: “Alternatively, it may be of increased importance to use screws with smaller diameters to limit the articular defect at the time of insertion. While this is a theoretical concern, there are currently no studies evaluating long-term degenerative changes following retrograde IMHS insertion.”
The study is limited by its retrospective nature. Dr. Allen also noted that there was not an even distribution of fracture patterns and demographics among the population. “Most fractures were in males with small finger metacarpal fractures, and therefore our findings may not be widely generalizable. We also did not include metacarpal neck or open metacarpal fractures, further limiting the applicability to other cases.” Finally, he noted, “The length of the intramedullary screw and specifically the distance that it bypasses the fracture site may be of importance, though we did not assess this variable in the present study.”
When asked about further areas of exploration based on these findings, Dr. Luther said, “This study prompts a question of what threshold screw diameter is necessary to prevent negative clinical outcomes. The study identified a threshold of 75 percent canal fill to prevent radiographic displacement, but patients with <75 percent canal fill did not experience negative clinical effects.” he called for future studies to evaluate smaller screw diameters “to determine the minimum diameter necessary to prevent adverse clinical outcomes,” as well as studies to validate concerns regarding long-term degenerative changes at the metacarpophalangeal joint due to articular defects made at the time of screw insertion.
Drs. Luther and Allen’s co-authors of “Effect of Screw Size on Radiographic and Clinical Outcomes in Metacarpal Shaft Fractures” are Alexander D. Jeffs, MD; Sarah Obudzinski, MD; Patricia Kirkland Wellborn, MD; and Zachary Visco, MD.
Rebecca Araujo is the managing editor of AAOS Now. She can be reached at raraujo@aaos.org.