A retrospective cohort study found that nicotine-dependent patients who underwent Achilles tendon repair had a significantly higher risk (P <0.05) of postoperative complications over a 20-year period than their non–nicotine-dependent counterparts.
For the study, researchers used TriNetX to evaluate de-identified patient information from 49 healthcare organizations and more than 93 million patients on the network in the United States. Achilles tendon repair was defined as a primary open or percutaneous repair or secondary repair with or without a graft. Two cohorts were evaluated for this study: Cohort A included patients who had an Achilles tendon repair and nicotine dependence, and cohort B included patients who had an Achilles tendon repair but did not have nicotine dependence. Patients with diabetes mellitus, gout, rheumatoid arthritis, and lupus were excluded from the analysis.
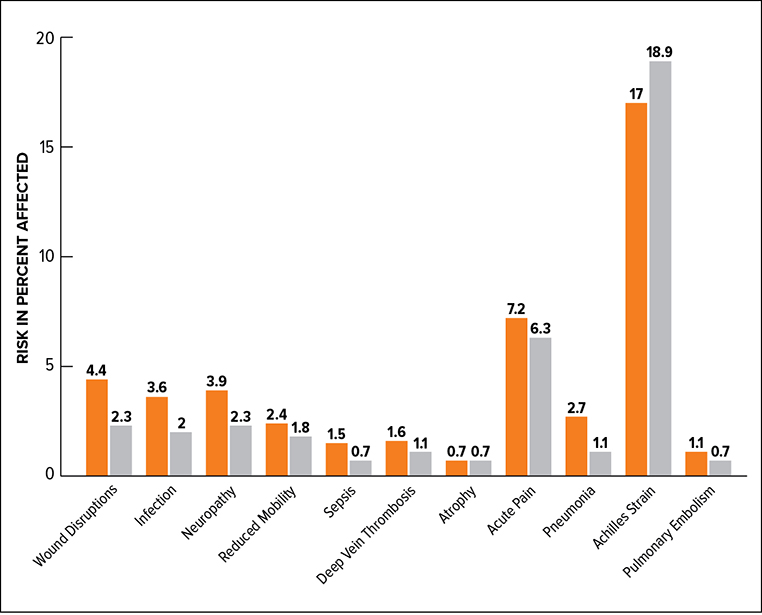
The cohorts were propensity matched for demographic factors such as age at event, ethnicity, race, and sex. Data were gathered from 2000 to 2023. The outcomes evaluated were wound disruption, infection following a procedure, mononeuropathy of the lower limb, reduced mobility, sepsis, deep vein thrombosis, atrophy, acute postoperative pain, pneumonia, Achilles tendon strain, and pulmonary embolism. All postoperative complications were analyzed 1 day to 5 years after Achilles tendon repair.
A total of 1,435 nicotine-dependent patients were matched with 14,056 non–nicotine-dependent patients. After propensity matching, the researchers found that nicotine-dependent patients who underwent Achilles tendon repair experienced higher risk for numerous postoperative complications. Compared with nondependent patients, nicotine-dependent patients had increased risk for wound disruption (P = 0.0477), infection following a procedure (P = 0.0179), mononeuropathy of the lower limb (P = 0.0029), sepsis (P = 0.047), and pneumonia (P = 0.0014) (Fig. 1).
Lead author Sterling J. DeShazo, medical student at University of Texas Medical Branch, said the apparent role of nicotine in causing complications was noteworthy. “This finding reinforced the fact that alternative nicotine devices may not be the best preoperative smoking alternative,” he told AAOS Now.
He said the study further supports the perioperative cessation of nicotine use and tobacco-related products due to their effects on postoperative complications. “Although the generalizability of our study is limited, this study serves as a marker to further evaluate perioperative cessation guidelines in the context of nicotine and other related products.”
For future research, Mr. DeShazo said a randomized, controlled trial relating nicotine usage and postoperative complications and/or outcomes would allow for “a much more significant and generalizable finding.” Future studies might also assess the efficacy of nicotine-replacement therapy versus smoking in the context of various orthopaedic surgeries.
Limitations of the study were misclassification and residual confounding that cannot be avoided when drawing from a large database that relies on administrative coding. Also, studies with a retrospective, observational design inherently have limited generalizability to a larger population, Mr. DeShazo noted. He added, “Even though we controlled for a number of confounding variables, our analysis control is limited and may not completely account for all patient characteristics.” Finally, he noted, “our data revolve around the ICD-10 code for nicotine dependence, which may be used differently from physician to physician, as it lacks specific, standardized definitions regarding dependence.”
Mr. DeShazo’s coauthor of “Nicotine Dependence Is Associated with Increased Rates of Postoperative Complications in Achilles Tendon Repair: A Propensity-Matched Comparison” is Vinod Kumar Panchbhavi.