Editor’s note: The following article is a review of a video available via the AAOS Orthopaedic Video Theater (OVT). AAOS Now routinely reviews OVT Plus videos, which are vetted by topic experts and offer CME. For more information, visit aaos.org/OVT.
Chondrosarcoma is the second most common malignant primary bone tumor. Despite the condition’s many subclassifications, “conventional” types account for more than 90 percent of all presentations and are typically found in adults aged 40 years or older. Imaging demonstrates lytic lesions with intralesional calcifications. Tumors are most often located in the pelvis (25 percent), proximal or distal femur, proximal humerus, distal tibia, or scapula. If in the pelvis, these tumors can cause bowel or bladder obstruction due to mass effect. Histological features differ among subtypes but commonly include varying grades of chondrocyte atypia and myxoid change. Management involves wide surgical resection for any cases that are grade II or higher or have pelvic lesions. Chemotherapy and radiation are not indicated due to treatment resistance. Among conventional chondrosarcomas, 5-year survival rates drop with increasing tumor grade due to high rates of local recurrence and distant metastasis.
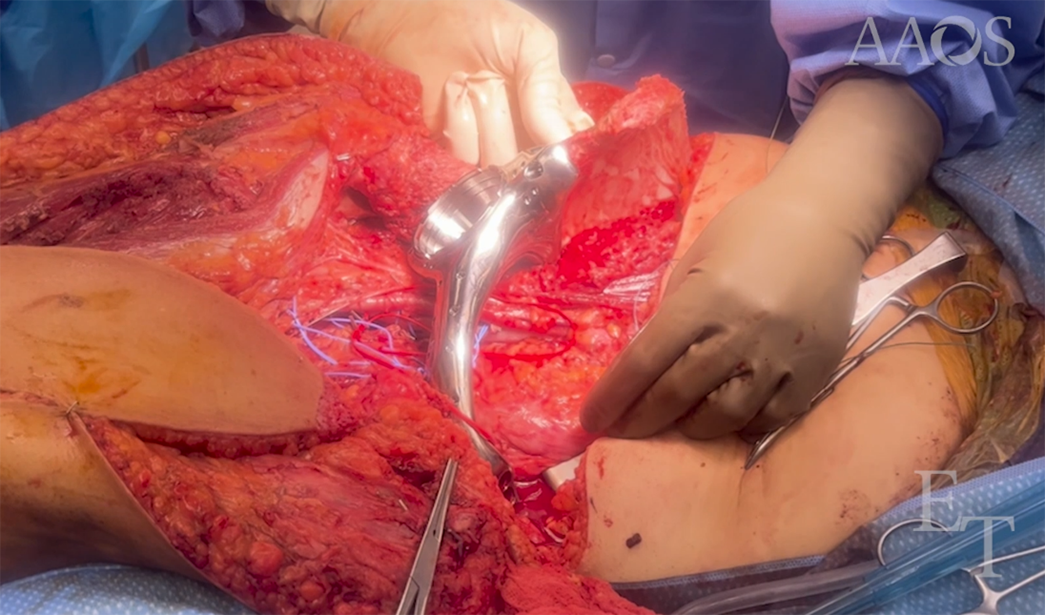
The AAOS OVT video titled “Hemipelvectomy for Chondrosarcoma with Custom Pelvic Reconstruction” demonstrates hemipelvic reconstruction after resection of a right-sided grade II chondrosarcoma involving the superior pubic rami, acetabulum, and soft tissues of the medial thigh. The patient had presented with an 8-month history of painful pelvic swelling, which had progressively migrated to her upper right thigh. A large firm mass was palpable along the right lower quadrant of the abdomen, and imaging confirmed a large lesion involving the superior pubic rami, anterior acetabulum, and medial compartment of the thigh.
The authors started with a thorough review of preoperative imaging and used a 3D CT scan to demonstrate their plan for resection. Given the extent of pelvic involvement, a custom pelvic implant and total hip arthroplasty were planned. The implant was to span from the ipsilateral iliac wing to the contralateral superior pubic rami.
A combined ilioinguinal and iliofemoral approach was used for the completion of right periacetabular and pubic rami and left pubic rami pelvic resection. A custom supra-acetabular cutting jig allowed for precise cuts and an excellent fit of the prosthesis to the right iliac wing. Screws at the most superior aspect of the implant’s flange were placed with eccentrically drilled holes to create compression at the iliac wing–implant interface. Two 6.5 mm hydroxyapatite-coated intramedullary screws were then applied for increased biologic fixation. These were aimed into the acetabular cup and up the anterior column. Screws were then placed into the contralateral rami. Lastly, a dual-mobility total hip arthroplasty was completed with a press-fit femoral stem. The plastics team performed a pedicled anterolateral thigh flap to help with coverage.
Postoperatively, the patient was placed on bed rest for one week before progressing to 50 percent weight bearing on the right lower extremity. She developed a foot drop, which was managed with an ankle foot orthosis. Wound complications required debridement and vacuum-assisted wound closure. She was discharged at 6 weeks after achieving full weight-bearing status. At the 6-month follow-up, the patient continued to ambulate well with a cane.
Overall, this video is a detailed and excellent presentation of a case involving an internal hemipelvectomy and subsequent reconstruction for a grade II periacetabular chondrosarcoma. It will be of high educational value to residents, fellows, and orthopaedic oncologists.
Michael DeRogatis, MD, MS, is an orthopaedic surgery resident at St. Luke’s University Health Network in Bethlehem, Pennsylvania, and serves as a resident member of the AAOS Now Editorial Board.
Neil Jain, MD, is a postdoctoral orthopaedic surgery research fellow at St. Luke’s University Health Network in Bethlehem, Pennsylvania.
Paul S. Issack, MD, PhD, FAAOS, FACS, is a clinical associate professor in the Department of Orthopaedic Surgery, Weill Cornell Medical College, and a trauma and adult reconstruction orthopaedic surgeon at New York–Presbyterian/Lower Manhattan Hospital. He is also a member of the AAOS Now Editorial Board.