Bone-health optimization (BHO) identifies patients who are at risk for osteoporosis for further assessment and, when indicated, appropriate treatment, as summarized in Table 1. Osteoporosis is associated with greater risk for complications and revision surgery. For example, periprosthetic fractures are frequently low-energy fractures in patients with osteoporosis. Subsidence of implants and loosening of fixation occur far more often in patients with poor bone stock. In spine surgery, bone-related complications have been reported in half of osteoporotic patients compared with 22.7 percent of patients with normal bone mineral density (BMD).
Current medical therapy for osteoporosis is very effective at increasing BMD and preventing fractures. Medical therapy also has a positive effect on preventing femoral bone loss after total joint arthroplasty and reducing implant subsidence. In spinal fusion, multiple randomized, controlled trials have demonstrated the benefits of bisphosphonate and anabolic treatment in osteoporotic patients compared to controls. Total joint registry studies have demonstrated an approximately 50 percent reduction in revision surgeries in patients treated with bisphosphonates. However, documentation of the effectiveness of BHO programs is lacking.
There are many barriers to introducing BHO into an orthopaedic clinic. Surgeons may be reluctant to add another burden to care flow, particularly when the condition is outside the comfort zone of their clinical expertise. Additionally, no standard has been accepted that identifies which patients need further assessment and treatment. Orthopaedic surgeons are not trained in the interpretation of dual-energy x-ray absorptiometry (DXA) scans and may be reluctant to order the test. Delays in obtaining diagnostic testing for osteoporosis and referrals to bone-health specialists are common. Ultimately, diagnosis and treatment of osteoporosis could lead to surgical delays, which may be poorly accepted by both the surgeon and the patient. The implementation of the fracture liaison service Own the Bone, proposed by the American Orthopaedic Association, can overcome many of these barriers.
Steps in preoperative BHO
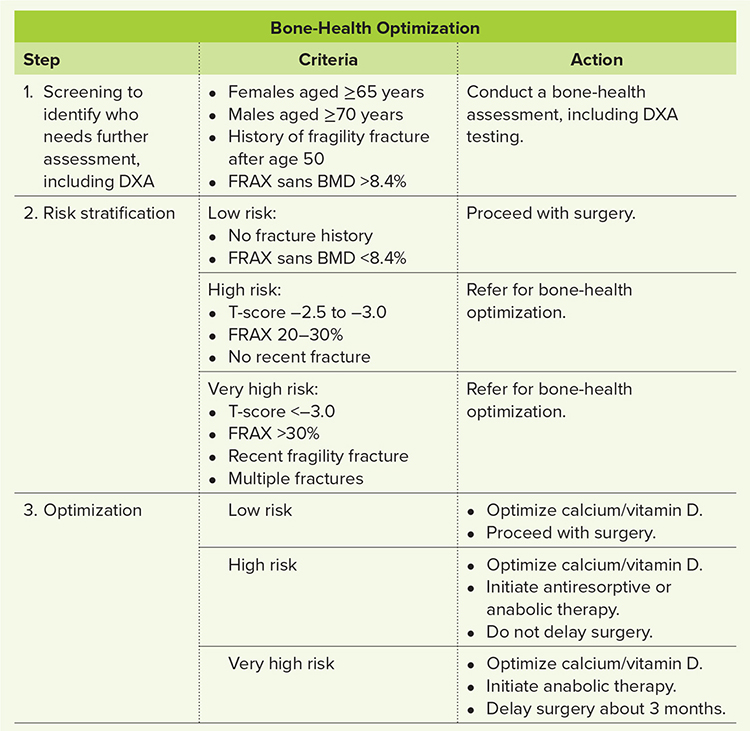
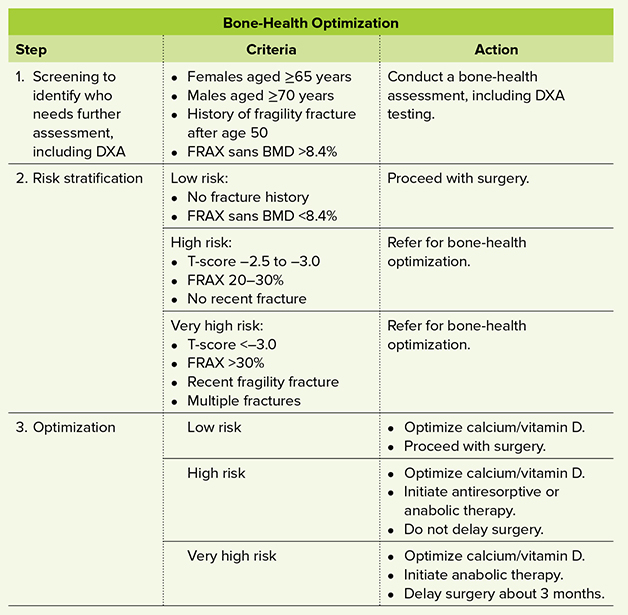
The first step in BHO is to identify which patients need further assessment, including BMD testing. The International Society for Clinical Densitometry has recommended that elective orthopaedic surgery patients undergo DXA testing if they are females aged ≥65 years or males aged ≥70 years, have a history of fragility fracture after 50 years of age, or have a Fracture Risk Assessment Tool (FRAX) score >8.4 percent. Note, not all patients need densitometry, only those who meet any of these criteria. In patients scheduled to undergo total knee arthroplasty, the sensitivity and specificity of these criteria in identification of who needs DXA and ultimately has osteoporosis have been reported as 100 percent and 54 percent, respectively.
The second step for patients undergoing DXA testing is to classify the severity of the disease. Using only BMD has limitations, as most patients with fragility do not have T-scores <–2.5. a newer definition of clinical osteoporosis has been recommended that includes patients with a t-score><–2.5, history of recent hip or spine fracture, and high frax (10-year risk of hip fracture>3 percent or major osteoporotic fracture >20 percent). Patients who did not require testing are considered low risk and should proceed with surgery. High-risk patients are those with a T-score between –2.5 and –3.0 or a FRAX risk of major osteoporosis fracture between 20 to 30 percent. Patients are considered very high risk if they have a T-score <–3.0 or frax>30% or have sustained a recent fragility fracture, multiple fractures, or fractures while on medical treatment. High- and very-high-risk patients are referred for further evaluation and medical treatment.</–3.0></–2.5,></–2.5.>
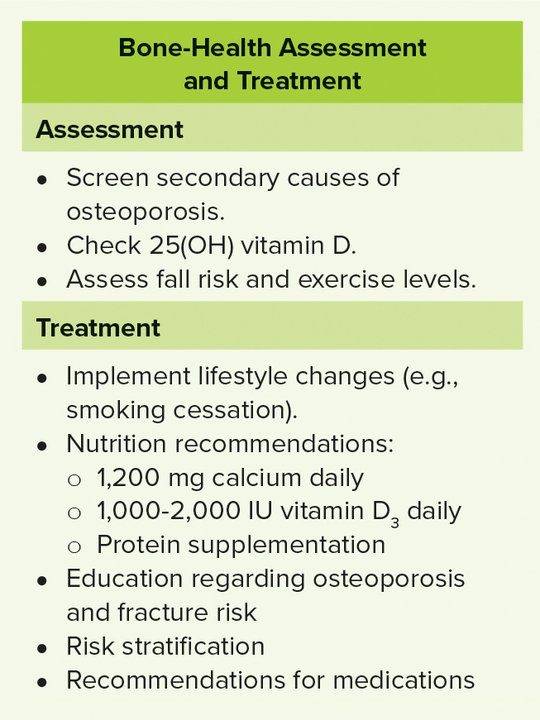
The third and final step in BHO is to refer patients for complete assessment and optimization. The process is similar to that after fracture and can be performed by orthopaedic surgeons and staff, primary care providers, or specialists such as endocrinologists. Many orthopaedic units have fracture liaison services capable of performing this function. A typical assessment is detailed in Table 2.
Medical management of osteoporosis includes recommendations for lifestyle changes, including discontinuation of tobacco products and excessive alcohol use; fall prevention (if indicated); correction of nutritional deficits (e.g., malnourishment, vitamin D deficiency); and correction of any modifiable, secondary osteoporotic conditions. High-risk patients are candidates for pharmacotherapy with either antiresorptive or anabolic therapy. The author prefers anabolic medication, as it increases BMD, reduces fracture risk, and causes measurable bone formation within 3 months.
Cost considerations, insurers’ reluctance, and potential off-label use may limit availability for some patients. Patients with severe osteoporosis meet criteria for anabolic therapy, such as parathyroid hormone analogs and romosozumab, which are indicated not only to improve surgical outcomes but also to reduce fracture risk.
Deciding whether surgical delay for BHO is warranted should be based on the severity of osteoporosis, the complexity of surgery, and the urgency. Unfortunately, little direct medical evidence is currently available on the impact of surgical delay. The author recommends a surgical delay of 3 months when initiating medical therapy for osteoporosis. However, if the surgical indications require urgent surgery, such as for a neurologic deficit or inability to ambulate due to severe hip arthritis, surgery should proceed and BHO should be performed postoperatively. For complex procedures requiring higher-quality fixation and large amounts of bone union, delays as long as 9 months are occasionally indicated.
BHO recognizes the important role of skeletal integrity in orthopaedic surgery. Surgeons should consider bone health during the evaluation phase prior to elective surgery by identifying patients at risk and using DXA testing when appropriate. If clinical osteoporosis is present, patients should be referred for further evaluation and treatment. Treatment may include medication and surgical delay.
Paul A. Anderson, MD, FAAOS, is a board-certified orthopaedic spine surgeon. He is an internationally recognized expert in the field of orthopaedic spinal surgery and emeritus professor of orthopaedics at the University of Wisconsin.
References
- Edwards PK, Mears SC, Stambough JB, et al: Choices, compromises, and controversies in total knee and total hip arthroplasty modifiable risk factors: what you need to know. J Arthroplasty 2018;33(10):3101-6.
- Dlott CC, Moore A, Nelson C, et al: Preoperative risk factor optimization lowers hospital length of stay and postoperative emergency department visits in primary total hip and knee arthroplasty patients. J Arthroplasty 2020;35(6):1508-15.e2.
- Anderson PA, Jeray KJ, Lane JM, et al: Bone health optimization: Beyond Own the Bone: AOA critical issues. J Bone Joint Surg Am 2019;101(15):1413-9.
- Bjerke BT, Zarrabian M, Aleem IS, et al. Incidence of osteoporosis-related complications following posterior lumbar fusion. Global Spine J 2018;8(6):563-9.
- Camacho PM, Petak SM, Binkley N, et al: American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis—2020 update. Endocr Pract 2020;26(Suppl 1):1-46.
- Anderson PA, Binkley NC, Bernatz JT: Bone health optimization (BHO) in spine surgery. Spine 2023;48(11):782-90.
- Anderson PA, Morgan SL, Krueger D, et al: Use of bone health evaluation in orthopedic surgery: 2019 ISCD official position. J Clin Densitom 2019;22(4):517-43.
- Chang E, Binkley N, Krueger D, et al: Proposed bone health screening protocol to identify total knee arthroplasty patients for preoperative DXA. Osteoporos Int 2023;34(1):171-7.