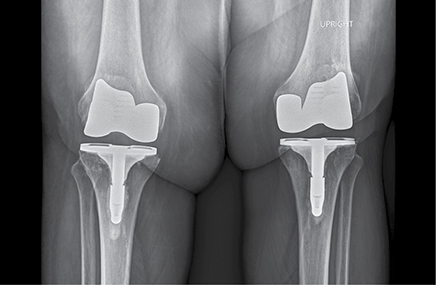
Morbid obesity (MO; BMI >40 kg/m2) is a known risk factor for complications in patients undergoing total knee arthroplasty (TKA), including increased risk of revisions and poorer outcomes. A study presented at the 2023 American Association of Hip and Knee Surgeons (AAHKS) Annual Meeting showed that using a tibial stem extension may help shield against MO-associated complications in patients undergoing TKA.
“Since we know there are higher failure rates in morbidly obese patients, we wanted to determine if the amount of load per square surface of the tibial baseplate can yield to forces that cause failure of the implant,” said Ran Schwarzkopf, MD, MSc, FAAOS, associate chief of the division of adult reconstruction, director of the adult reconstruction research center, and professor of orthopaedics at NYU Langone Orthopedic Hospital. “Adding a longer stem can potentially abate the increased force and decrease the amount of failure. This could help us figure out if we should and could treat obese patients differently through a small stem extension.”
The retrospective cohort study included 750 patients with MO older than 18 years who underwent primary, elective TKA at a single academic center and received either a keel-only (KO; 699 patients) tibial component or a tibial component with a keel and a stem extension (keel and stem, KS; 51 patients). Outcomes included operative time, length of stay, 90-day emergency department visits, 90-day hospital readmissions, all-cause revisions, revision indications, and implants revised. The Knee Injury and Osteoarthritis Outcome Score for Joint Replacement (KOOS JR) was used for evaluation, and the researchers compared scores preoperatively and 3, 6, and 12 months postoperatively.
Patients who had a KO TKA had higher rates of all-cause revisions (3.9 versus 12.4 percent; P = 0.069) and tibial component revisions (2 versus 8 percent; P = 0.115), but this was not statistically significant. Of two revisions in the KS group, one patient developed an infection and underwent revision and one patient was revised for mechanical instability. In the KO group, one patient was revised for instability (1.1 percent), one for component malposition (1.1 percent), three for periprosthetic fracture (3.4 percent), nine for arthrofibrosis (10.3 percent), 18 for mechanical instability (20.7 percent), 26 for infection (29.9 percent), and 29 for aseptic loosening (33.3 percent). Of the revisions for aseptic loosening, 23 of 29 patients (79.3 percent) were indicated for revision due to tibial component loosening.
The 5-year survival from both all-cause revision (86.7 percent versus 96.1 percent; P = 0.229) and tibial component revision (90.8 percent versus 98.0 percent; P = 0.303) also showed increased revision rates in the KO group. Patients in the KS group reported significantly higher KOOS JR scores one year after surgery (68 versus 63; P = 0.047), although significance was not achieved at any other point in time.
BMI and weight were associated with an increased risk of tibial component revision. The risk analysis found that 118 kilograms (260 pounds) was an optimal cutoff weight to reduce the risk of aseptic loosening and tibial component revision, especially in the KO patients. The rate of tibial component revision in the KO cohort was 16 percent for patients who weighed more than 118 kilograms compared to 9.9 percent for those below 118 kilograms. This suggests that a tibial stem extension may increase the longevity of tibial components through the dispersion of forces on the baseplate. The difference was similar above or below the 118-kilogram cutoff weight in the KS group.
Dr. Schwarzkopf explained, “Our study showed that by adding a short stem extension to the tibial baseplate in morbidly obese patients, we see a decrease in revision rates. This led us to look more in depth, not just at the BMI cutoff, but also at the weight cutoff since BMI is a relationship between weight and height and doesn’t truly reflect the amount of force that the baseplate experiences. We are currently looking at the exact size of the tibial baseplate for each patient and correlating the patient weight so it can actually calculate the exact weight per surface area. This may help us provide better recommendations outside just a pure BMI or weight cutoff.”
The study did have a few limitations, including being retrospective and, therefore, vulnerable to selection bias. This also limited the ability to establish causality between the type of tibial component and outcomes. Additionally, follow-up data were limited to one institution, so any surgeries or follow-up at other institutions were unattainable. Comorbidities were not included in this study, which can affect outcomes.
Dr. Schwarzkopf’s co-authors of “Do Stemmed Tibial Components Improve Outcomes for Patients with BMI >40 Undergoing Primary Total Knee Arthroplasty?” are Spencer A. Ward; Itay Ashkenazi, MD; Akram A. Habibi, MD; Neel Vallurupalli; Claudette M. Lajam, MD, FAAOS; and Joshua C. Rozell, MD.
Molly Todd Rudy is a freelance writer for AAOS Now.