Segmental bone defects in the context of trauma, infection, or reconstruction are a challenge to the orthopaedic surgeon and patient no matter the training or expertise. There are numerous available strategies to address bone defects, and each has its own unique benefits and drawbacks that drive the choice of management. Other factors driving decision making are the surgeon’s skillset, availability of resources (both from the patient and the hospital), and patient preference. Unfortunately, no “gold standard” technique exists, and direct comparison has not historically been performed due to the unique nature of each defect.
For several years, the three primary options that were available to orthopaedic surgeons treating segmental defects were external fixation using Ilizarov principles; the induced membrane technique, also known as the Masquelet technique; and vascularized bone grafts. However, more contemporary treatment of bone defects involves a variety of techniques that capitalize and expand on many of the lessons learned from earlier techniques.
Induced membrane “Masquelet” technique
The induced membrane technique, which was introduced in the 1980s by Alain-Charles Masquelet, has gained significant popularity, with hundreds of papers published since its inception. Many surgeons are familiar with the technique, which involves resection of bone and placement of a cement spacer followed by waiting for at least 4 weeks for a membrane to develop. The patient later returns to have the spacer removed, and bone grafting of the defect is performed. Up to a 90 percent success rate has been reported.
The technique benefits from being all internal, not requiring frequent visits to the clinic, and being a relatively easy procedure to perform. However, the definition of success is variable, and patients often require repeat trips to the OR for additional bone grafting or other procedures due to complications such as fracture of incomplete union or donor-site complication. Modern implementation of the technique involves the usage of commercially available scaffolds, including both titanium and bioabsorbable polymers. These enhancements have been designed to limit some of the complications associated with the technique; however, reports of their use in clinical series are limited.
External fixator bone transport
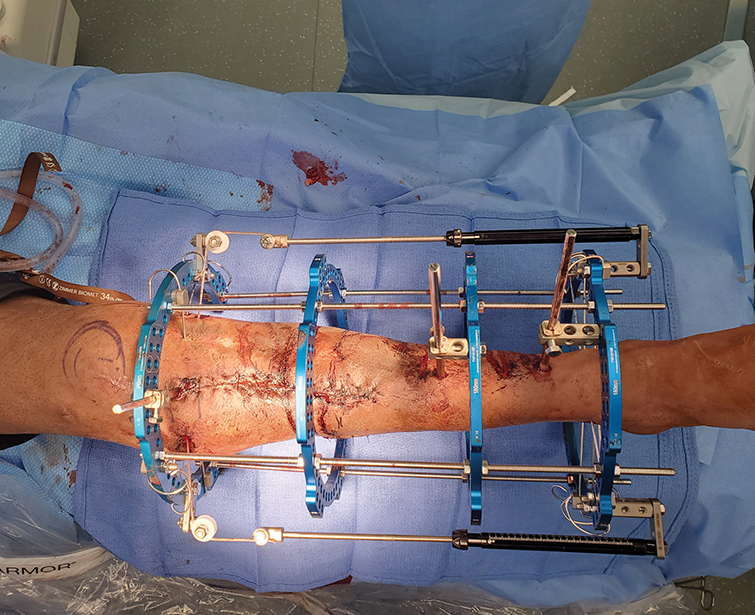
Bone transport, which historically was performed via the use of ringed external fixators (sometimes rail-type fixators), now represents a family of techniques that capitalize on Gavriil Ilizarov’s concept of distraction osteogenesis, that is, performing an osteotomy (or a corticotomy as Ilizarov described) distant from the defect site and slowly transporting the intact bone segment into the defect while leaving new bone or regenerate in its wake. Performance of this technique using external fixation, although often successful (up to 95 percent), comes at a cost to the patient and care team, including pain, long-lasting psychological effects, complications associated with indwelling pins, pain, loosening of components, and frequent visits to the clinic.
Ring fixation bone transport has been further improved by removing the need for wires/pins that traverse the skin/soft-tissue envelope, which can result in an unpleasant experience for the patient or poor cosmetic results. Cable transport, which utilizes an indwelling stranded cable to pull the transport segment into the bone defect while using the frame as a scaffold, improves the patient experience tremendously (Fig. 1). Balanced cable transport, as recently described by Quinnan et al., allows for the management of large defects and can be accomplished with multiple osteotomies to decrease the time required to be in the frame even further. Additionally, the combination of this technique with transition to an intramedullary nail can minimize the time in frame from months to a matter of weeks. Although its use can be complex, surgeons familiar with Ilizarov techniques can learn the skill easily.
As time in the external fixator increases, the risk of difficulties increases, including pin-site infections, loosening, pain, and frame fatigue. Contemporary usage of external fixators minimizes the length of time spent in the frame by transitioning to internal nails after the “work” has been done via the external fixator. This can be accomplished either by placing the intramedullary nail at the time of fixation via the so-called “lengthening over a nail” technique or via placing the nail after external fixation via the so-called “lengthening and then nailing” technique. These techniques dramatically reduce the required time in the frame, improving the patient experience. Concerns regarding infection at pin sites are mitigated via out-of-plane wires/pins, pin-site holidays, and deposition of calcium sulfate laden with antibiotics prior to nail placement.
All-internal bone transport
In the recent past, all-internal bone transport was described by Barinagaet al. and Olesen et al. using the plate-assisted bone segment transport (also called PABST) technique. The technique combines the use of standard fracture fixation plates with motorized lengthening nails. Essentially, the fracture fixation plate functions as a scaffold akin to the external fixator while the limb lengthening nail pushes or pulls the transport segment.
The benefits of this technique are that it is all internal and very well tolerated. However, the technique necessitates a healthy soft-tissue envelope and a bone defect which is amenable to the technique. These limitations are dictated by the implants used, as well as the size and location of the defect (e.g., very proximal or distal defects may not be stabilized by the implant). The technique, although powerful, is technically demanding and may require adjustment when the defect is closed (mismatch of trajectory of lengthening nail and anatomically contoured plate). Additionally, issues with hardware failure and loss of fixation can occur.
The internal bone transport nail represents the most recent development in this arena, with a nail that can accomplish all aspects of bone transport without a supplemental plate or external fixator. The bone transport nail, released by NuVasive Orthopaedics, is a promising device that revolutionizes bone-defect management. The implant allows for all-internal bone transport using standard nailing techniques, which many surgeons are familiar with. Its use was well tolerated by patients and was only limited by the geometry of the nail and the size of the defect. Unfortunately, the device was voluntarily recalled from the market prior to widespread adoption due to reports of corrosion upon implant removal. The manufacturer has plans to release a new version of the nail in the future.
Historically, shortening an extremity for the purpose of defect management has not been popular due to the inherent consequences of a shortened extremity. However, with the advent of modern internal lengthening methods, such as motorized lengthening nails, acute shortening can be a favorable option to help close open wounds and manage segmental defects. As part of a staged procedure, once the segment has healed, the surgeon can return at a later date to electively lengthen the extremity. However, even shortening has its limits. Soft tissues, including neurovascular structures, have a limit to how much they can be shortened, which can result in consequences such as loss of blood flow (kinking of vessels). This technique is often relegated to situations where shortening the extremity aids in wound closure and is preferable to some type of tissue transfer.
Contemporary treatment of bone defects continues to evolve and has drastically changed within the past 10 to 20 years. Modern techniques involve decreasing the need for an external fixator, decreasing complexity, and improving the patient experience. No one technique can address all defects. Choice of the technique depends on the surgeon’s familiarity, characteristics of the defect, availability of resources, and patient preference.
Paul E. Matuszewski, MD, is an associate professor of orthopaedic traumatology and chief of the orthopaedic trauma service at the University of Kentucky. In addition to trauma, he specializes in limb lengthening, deformity correction, and the treatment of osteomyelitis. He serves as an executive board member of the Limb Lengthening and Reconstruction Society.
Stephen Quinnan, MD, is a clinical professor of surgery at Florida Atlantic University and serves as both chief of orthopaedic trauma and head of the Amputee Optimization Program at the Paley Orthopedic and Spine Institute at St. Mary’s Medical Center in West Palm Beach, Florida. He is also director of orthopaedic research and education at St. Mary’s. Dr. Quinnan currently serves as the president of the Limb Lengthening and Reconstruction Society.
Mani Kahn, MD, MPH, is an assistant professor, chief of the orthopaedic trauma division, and orthopaedic surgery residency program director at Albert Einstein College of Medicine in Bronx, New York. He specializes in trauma and limb deformity at Montefiore Medical Center in the Bronx. Dr. Kahn serves on the executive board of the Limb Lengthening and Reconstruction Society.
References
- Quinnan SM, Lawrie C: Optimizing bone defect reconstruction-balanced cable transport with circular external fixation. J Orthop Trauma 2017;31(10):e347-55.
- Rozbruch SR, Kleinman D, Fragomen AT, et al: Limb lengthening and then insertion of an intramedullary nail: a case-matched comparison. Clin Orthop Relat Res 2008;466(12):2923-32.
- Paley D, Herzenberg JE, Paremain G, et al: Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am 1997;79(10):1464-80.
- Barinaga G, Beason AM, Gardner MP: Novel surgical approach to segmental bone transport using a magnetic intramedullary limb lengthening system. J Am Acad Orthop Surg 2018;26(22):e477-82.
- Olesen UK, Nygaard T, Prince DE, et al: Plate-assisted bone segment transport with motorized lengthening nails and locking plates: a technique to treat femoral and tibial bone defects. J Am Acad Orthop Surg Glob Res Rev 2019;3(8):e064.
- Blair JA, Puneky GA, Swaminathan N, et al: Tibial bone transport with a single implant all-internal bone transport nail. J Orthop Trauma 2023;37(7):e294-300.