The debate persists over hemiarthroplasty versus total hip arthroplasty (THA) for displaced femoral neck fractures in older patients, as there are concerns that hemiarthroplasty can lead to acetabular wear, which can then lead to poorer functional outcomes. Various studies have shown that THA in elderly, active patients led to better patient-reported outcome scores. The argument against THA in fracture patients has been the higher risk of dislocation compared with hemiarthroplasty, but newer dual-mobility femoral head options may mitigate that risk. The AAOS Clinical Practice Guideline on Management of Hip Fractures in Older Adults provides a moderate-strength recommendation for THA in patients with displaced femoral neck fractures, as the functional benefit is higher.
Does this shift in improved medical status and expectation for better function require orthopaedic surgeons to alter hip fracture treatment? Hence, the idea of “traumaplasty” arises—a blend of trauma surgery and joint arthroplasty.
Consider the following clinical scenario: A healthy 80-year-old woman presented to the ED with a displaced femoral neck fracture following a pickleball injury. The highly experienced orthopaedic trauma surgeon on call evaluated her and discussed hemiarthroplasty. The surgeon called the patient’s prior orthopaedic surgeon, stating that he was comfortable with hemiarthroplasties but had done very few THAs in residency. Given her high level of function and evidence that THA has better results in a similar population, he asked her previous surgeon to assume care. The surgeon then performed a THA, after which the patient did well.
Suppose this patient had presented elsewhere where the on-call orthopaedic surgeon was not comfortable with THAs and there was no arthroplasty colleague available. Would this patient have undergone hemiarthroplasty, which is still within standard of care, even though recent data show superior outcomes with THA in this population? Should orthopaedic surgery departments consider having a traumaplasty service to address cases such as this example?
There are several areas of consideration regarding a traumaplasty service. First is volume: Hip fractures in older patients are common orthopaedic injuries. Femoral neck fractures represent a significant proportion of hip fractures With advances in medical care, older patients are surviving longer with higher demands for mobility. Just as fracture care evolved from casts and splints to rigid internal fixation for better outcomes in selected cases, hip fracture will need to evolve to meet the demands of patients with longevity.
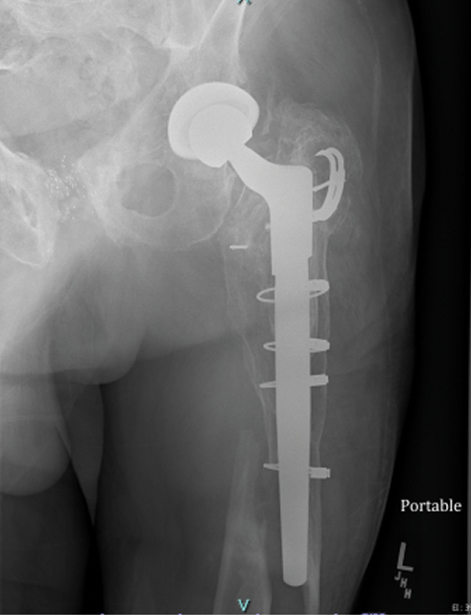
The second consideration of a traumaplasty service is periprosthetic fractures. Given the rising demand for total joint replacement, as well as life expectancy, older patients are leading more active lives. In turn, periprosthetic fracture rates are rising. Total joint replacement surgeons and orthopaedic trauma surgeons may be called upon to manage acute periprosthetic fractures (Fig. 1).
The third aspect of traumaplasty is management of failed fracture fixation necessitating joint replacement (e.g., three screws used for fixation of a hip fracture, with subsequent development of osteonecrosis or femoral head collapse) (Fig. 2). These procedures are not the same as primary total joint replacements with hardware removal. Although these cases are not necessarily emergent procedures, they are not completely elective either, due to not only the level of pain and disability but also concerns about hardware (e.g., screws) eroding into the acetabulum, leading to significant loss of bone stock. This complication requires expedited scheduling of procedures, with medical optimization. In addition, the surgeon needs to have appropriate equipment, such as proprietary screwdrivers and hardware-removal equipment specific to the manufacturer of the failed implant. Depending on the amount of bone loss, revision-type hip arthroplasty implants may be needed, such as calcar-replacing long-stem femoral components. It is imperative that hospitals and insurers understand that these types of procedures are not simply primary THAs that can necessarily be managed with conventional primary implants.
Practice considerations
A traumaplasty service requires the on-call orthopaedic surgeon to have skills in both the trauma and arthroplasty realms. The arthroplasty surgeon needs skills in orthopaedic trauma care when faced with a periprosthetic fracture. The orthopaedic trauma surgeon needs skills in arthroplasty when addressing a displaced femoral neck fracture. The orthopaedic trauma surgeon needs skills in arthroplasty when addressing a displaced femoral neck fracture. When patients come to the ED with a femoral neck fracture, they expect to receive high-quality, evidence-based care, regardless of the luck of the draw of who is on call. Recognizing that patients require acute THA as the best option for care, based on current evidence, do hospitals and health systems have the resources to offer this service? There are several factors to consider when answering this question.
Implant availability is one consideration, as inventory and shelf space are often limited in hospitals. OR time and personnel are additional considerations. THA requires additional steps, equipment, and staff who are familiar with the technique. In community settings, availability of surgical assistants may be limited, making THA challenging.
Cost is also an important factor. Inserting an acetabular component incurs additional costs. Furthermore, some hospitals have contract restrictions that limit which types of acetabular cups and femoral stems are available. Osteoporotic fractures may require a specialized acetabular cup with multiple screw holes and higher friction fit. However, some hospital systems restrict the use of these types of acetabular cups to revision hip arthroplasties and do not permit their use in primary THA, even in the setting of severe osteoporosis. Regarding bone cement, data have shown a reduced risk of periprosthetic fractures and revisions with cemented arthroplasties for femoral neck fractures; however, there are concerns about costs in addition to the rare complication of bone cementation implantation syndrome.
Another practice consideration is surgeon availability. Depending on a hospital’s setup, on-call duties for the ED may be relegated to orthopaedic trauma surgeons. General orthopaedic surgeons may or may not participate in the panel. Although they have had general orthopaedic training and are comfortable performing hemiarthroplasties for femoral neck fractures, general or trauma surgeons may not have expertise in THA. Therefore, this procedure falls to the arthroplasty surgeon, who must find OR time to perform the surgery. The surgery may need to be done after-hours or require cancellation of clinic patients. Additionally, arthroplasty surgeons may not receive compensation to provide emergency care, as they were technically not on call for the ED, even though they were referred patients from the on-call trauma surgeon.
Will hospitals need to consider a dedicated hip fracture service (as some do already) to include a panel of surgeons comfortable with total joint replacement?
Surgeon considerations
When treating patients with periprosthetic fractures, are the orthopaedic surgeons taking ED call prepared?
- It may be necessary to revise loose prosthetic components. Should orthopaedic trauma surgeons be expected to manage this?
- As these fractures are often complex, there is a need to have specialized plates, screws, cerclage wires, and precontoured plates.
- If the prosthetic implants need to be removed, specialized implant-removal systems may be necessary.
Should surgeons taking general orthopaedic trauma call receive training in THA, and should arthroplasty surgeons have additional skills in fracture care? With regard to training programs, should residency programs be expected to provide training for performing THAs for acute femoral neck fractures and not just hemiarthroplasties?
For surgeons providing coverage to the ED and having to treat hip fractures and periprosthetic fractures, the author would suggest:
- If a total hip replacement is indicated in a community ambulator with a displaced femoral neck fracture, surgeons should collaborate with arthroplasty colleagues if they are not comfortable with THA.
- To manage periprosthetic fractures, surgeons must ensure that they have had training and experience with fixation. If components need to be revised, surgeons who are not revision surgeons should ask for help.
- Training programs may want to consider adding competencies for primary THA for fracture.
Collaboration is necessary, and health systems will need to allocate resources and compensation to provide the highest quality of care that orthopaedic patients deserve.
Rina Jain, MD, FRCSC, is a board-certified orthopaedic surgeon with arthroplasty fellowship training. She takes general orthopaedic call for a local hospital, which is a level 1 trauma center.
References
- Liu Y, Chen X, Zhang P, Jiang B: Comparing total hip arthroplasty and hemiarthroplasty for the treatment of displaced femoral neck fracture in the active elderly over 75 years old: a systematic review and meta-analysis of randomized control trials. J Orthop Surg Res 2020;15(1):215.
- Swenning T, Leighton J, Nentwig M, Dart B: Hip fracture care and national systems: the United States and Canada. OTA Int 2020;3(1):e073.
- Frisch NB, Wessell N, Charters M, et al: Hip fracture mortality: differences between intertrochanteric and femoral neck fractures. J Surg Orthop Adv 2018;27(1):64-71.
- Guyen O: Hemiarthroplasty or total hip arthroplasty in recent femoral neck fractures? Orthop Traumatol Surg Res 2019;105(1S):S95-101.
- Singh JA, Yu S, Chen L, Cleveland JD: Rates of total joint replacement in the United States: future projections to 2020-2040 using the National Inpatient Sample. J Rheumatol 2019;46(9):1134-40.
- Pivec R, Issa K, Kapadia BH, et al: Incidence and future projections of periprosthetic femoral fracture following primary total hip arthroplasty: an analysis of international registry data. J Long Term Eff Med Implants 2015;25(4):269-75.