Osteoporosis affects more than 12 percent of adults 50 years of age or older in the United States, and 43 percent of adults of this same demographic have osteopenia. Low bone mineral density (BMD), the defining characteristic of osteoporosis and osteopenia, affects more than half (55 percent) of older adults, who are at risk for fragility fractures.
Fragility fractures can occur from relatively low-energy injuries and can include distal radius fractures, vertebral fractures, and hip fractures. These fractures result in decreased function and are also associated with a higher risk of mortality. Fragility fractures are estimated to occur in 40 percent to 50 percent of women and 13 percent to 22 percent of men in their lifetimes, accounting for as much as $19 billion in healthcare costs each year.
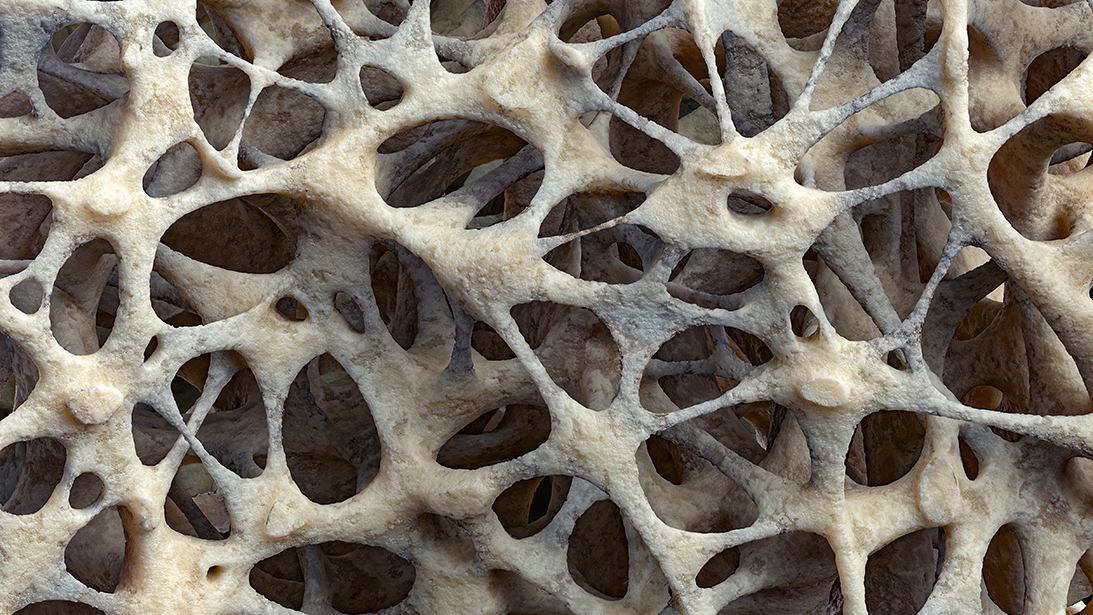
In addition to increasing the risks and morbidity of fragility fractures, poor bone health can be an important factor in preoperative evaluation of patients undergoing orthopaedic surgery. For example, studies have shown that as many as 25 percent of total joint arthroplasty patients meet criteria for pharmacologic osteoporosis treatment. The presence of osteoporosis can affect outcomes in orthopaedic surgery by increasing risk of intraoperative fractures, periprosthetic fractures, and hardware or implant loosening—ultimately contributing to a higher rate of complications and revision surgeries.
Management of osteoporosis includes lifestyle modifications and pharmacologic treatment with drugs that inhibit bone resorption or stimulate bone formation, such as bisphosphonates, raloxifene, denosumab, and estrogen. An understanding of the diagnosis and pathways for osteoporosis management can help orthopaedic surgeons in preoperative planning. Additionally, the first presentation of a patient with osteoporosis is often to an orthopaedic surgeon for treatment of a fragility fracture.
The gold standard for diagnosis of low BMD, including osteoporosis and osteopenia, is the dual x-ray absorptiometry (DXA) scan. DXA scans are informative; however, they carry several disadvantages, including variability of results based on factors such as presence of degenerative disease and overlying tissue artifact. Given these limitations, other imaging modalities have been studied as alternatives to DXA scanning in the diagnosis of osteoporosis. These include plain radiographs of the upper extremity, CT imaging of the wrist and spine, MRI, and quantitative ultrasound of the calcaneus. Finally, clinical assessment tools use clinical factors to help predict risk of osteoporosis and fracture, such as age, sex, previous fracture, smoking, alcohol use, and steroid use.
An abundance of clinical instruments have been developed, including the Fracture Risk Assessment Tool (also known as FRAX), Garvan Fracture Risk Calculator, Osteoporosis Self-Assessment Tool, Osteoporosis Risk Assessment Instrument, Simple Calculated Osteoporosis Risk Estimation instrument, Fracture and Immobilization Score, QFracture, Fracture Risk Score, Male Osteoporosis Risk Estimation Score, and Osteoporosis Self-Assessment Tool for Asians. Studies of these instruments have found variable accuracy, including variations based on gender and location of predicted fracture.
Despite the significant consequences and prevalence of osteoporosis, bone health screening remains poorly utilized in practice. The U.S. Preventive Services Task Force (USPSTF) currently recommends screening for osteoporosis in women aged 65 years or older and in younger women with equal or greater risk. Recommendations on intervals between testing vary from 2 to 10 years, depending on age, baseline BMD, and other risk factors. There are currently no USPSTF guidelines for men, although other groups, including the Bone Health and Osteoporosis Foundation, recommend screening in men aged 50 years and older with a fragility fracture. However, it is estimated that bone density screening is performed in less than 25 percent of patients in whom DXA screening is recommended. Specifically, there continue to be low rates of BMD screening following fragility fracture. For example, estimates suggest that only 10 percent to 20 percent of patients with distal forearm fragility fractures subsequently underwent BMD testing within 1 year of the fracture. Overall, significant gaps remain in care pathways and populations selected for BMD screening. Systems-based factors such as difficulties with coordination of care, patient insurance, and patient and clinician education about screening may contribute to these low rates.
Plain hand radiographs have emerged as a promising tool in screening for osteoporosis and osteopenia. Because osteoporosis is thought to affect the entire skeleton, changes in BMD can alter cortical bone thickness in the hand. Specifically, the second metacarpal cortical percentage (2MCP) on hand radiographs (calculated as the ratio of cortical diameter to total diameter at the isthmus on a posteroanterior view) has been correlated with hip BMD from DXA scans. The 2MCP method has been validated across studies to predict both osteoporosis and osteopenia. Clinicians should consider initiating treatment, or at least further BMD testing, in patients with 2MCP less than 60 percent. Conversely, DXA screening may be unnecessary in patients with 2MCP greater than 65 percent, which may help clinicians use resources more efficiently. Advantages of hand radiographs include its availability, accessibility, and low cost. Calculating 2MCP is relatively simple, requires minimal time, and can identify patients for additional screening. Other studies have also found correlations between BMD and cortical thickness of other bones in the appendicular skeleton, such as the distal radius, clavicle, and humerus.
In the past few years, advances in artificial intelligence (AI) have demonstrated the ability of machine learning to automatically calculate 2MCP from a hand radiograph, predicting osteoporosis from hand radiographs using 2MCP as a proxy measure. These recent findings demonstrate the promise of AI to automate screening for osteoporosis on imaging. Successful utilization of automated screening through radiographs could allow for dramatic expansion of screening for more patients.
Continued efforts to improve care pathways, screening recommendations, and diagnostic tools will be necessary to expand screening and treatment of patients with osteoporosis and osteopenia. Patient and clinician education on indications for screening and streamlining of referral pathways may help with rates of screening in at-risk populations. With rapid advances in AI, integration of automated tools in the clinical workflow may dramatically alter clinical practice. These technological advances may also help to improve accessibility of screening. Future research directions may assess the impact of AI on patient screening rates, outcomes and effects on morbidity and mortality, and overall healthcare system and patient costs.
Anna Luan, MD, MS, is an assistant professor of plastic and reconstructive surgery at Stanford University Medical Center in Stanford, California.
Jeffrey Yao, MD, is a professor of orthopaedic surgery at Stanford University Medical Center in Stanford, California. He is currently director of the hand and upper-limb fellowship at the Robert A. Chase Hand and Upper Limb Center at Stanford University Medical Center.
References
- Schultz K, Wolf JM: Emerging technologies in osteoporosis diagnosis. J Hand Surg Am 2019;44(3):240-3.
- Schreiber JJ, Kamal RN, Yao J: Simple assessment of global bone density and osteoporosis screening using standard radiographs of the hand. J Hand Surg Am 2017;42(4):244-9.
- Burton H, Bodansky D, Silver N, Yao J, Horwitz M: Assessing bone mineral density using radiographs of the hand: a multicenter validation. J Hand Surg Am 2023;48(12):1210-6.