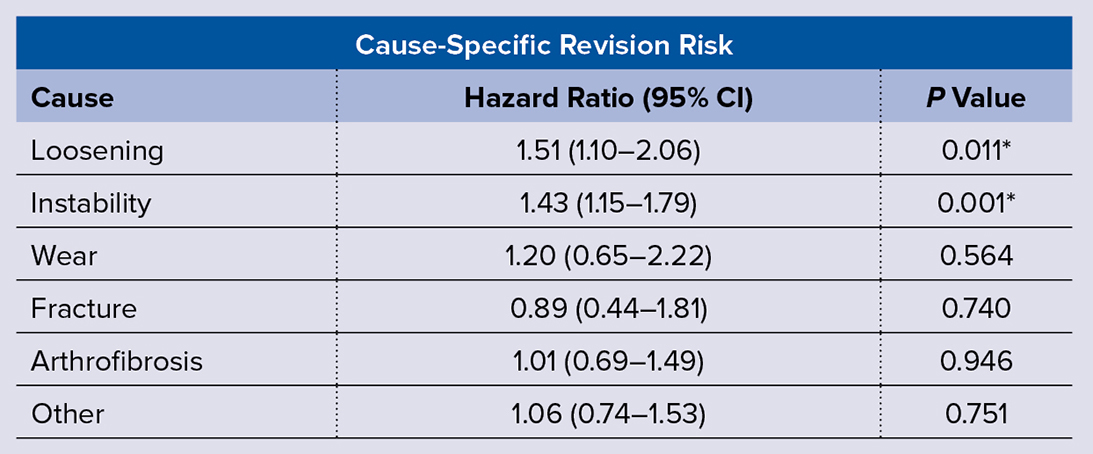
* indicates statistical significance CI, confidence interval
Newer-generation implants in total knee arthroplasty (TKA) were not found to improve risk of aseptic revision compared with older-generation implants, according to a study presented at the AAOS 2024 Annual Meeting. Matthew P. Kelly, MD, FAAOS, orthopaedic surgeon with Kaiser Permanente, presented the findings.
The study analyzed revision outcomes after TKAs performed with implants from a single manufacturer, comparing outcomes between a newer generation and an older generation. Data were gleaned from a U.S.-based total joint replacement registry.
Adult patients who underwent fully cemented TKA for osteoarthritis between 2009 and 2021 were included. The cohort included 47,869 patients who received the newer-generation system and 39,474 patients who received the older-generation system.
According to Dr. Kelly, the researchers sought to evaluate “if evolutionary design changes made any impact, for better or worse, on implant survivorship.” Overall, he concluded, “The newer implant designs did not confer better survivorship.”
Multivariable Cox regression was utilized to assess cause-specific aseptic revision risk, controlling for age, sex, BMI, race/ethnicity, American Society of Anesthesiologists physical status classification, bilateral procedure, cement viscosity, implant stability, and surgeon volume. Table 1 lists the hazard ratios (HRs) for overall risk of revision of the newer-generation implant system.
Overall, the newer implant systems had a significantly greater risk of revision for loosening and instability. “We were surprised somewhat by the increased risk for instability,” Dr. Kelly commented. “With greater sizing and poly thickness options, we were expecting there to be less instability in the newer designs.” There were no other differences in overall risk of revision for other causes, including wear, fracture, and arthrofibrosis.
When stratifying for implant constraint, “We saw an increase in aseptic revision overall for posteriorly stabilized (PS) and ultra-congruent (UC) TKA, which was significant for the reasons of loosening and instability,” Dr. Kelly noted. “When looking more closely at specific designs, the higher risk of TKA loosening was seen only with PS TKA, while the higher risk of instability was seen across the board with PS, UC, and cruciate-retaining (CR) TKA designs.”
For newer-generation PS implants, the HR for loosening was 1.44 (95 percent confidence interval [CI], 1.01–2.07; P = 0.046) and for instability was 1.33 (95 percent CI, 1.05–1.70; P = 0.020). Newer-generation CR implants had a higher risk of revision for instability (HR = 2.00; 95 percent CI, 1.13–3.52; P = 0.017) and newer-generation UC implants had a greater risk of revision for instability (HR = 2.17; 95 percent CI, 1.15–4.09; P = 0.016) compared with older-generation CR implants.
Regarding limitations, Dr. Kelly said, “As the study is observational, only associations are reported, not causality. There is potential for residual confounding due to unmeasured factors. For example, surgeons may have elected to use a specific implant stability based upon specific unmeasured patient characteristics.”
He noted that the authors attempted to mitigate this selection bias through stratification, also excluding fixed-bearing and constrained devices to minimize confounding due to implant attributes. Thus, the authors wrote, “The present results may not be generalizable to these types of devices.”
Additionally, “Our primary outcome was revision surgery. Other outcomes that may be of interest to the surgeon, including radiographic findings and patient-reported outcome measures, are not collected by the registry and therefore could not be evaluated,” he said. He called for further research to clarify the relationship between implant generation and other clinically relevant outcomes.
Paper 083 was presented on Tuesday.
Dr. Kelly’s coauthors of “Higher Aseptic Revision Risk following Primary Total Knee Arthroplasty for a Newer Generation Implant System Compared to Its Predecessor from the Same Manufacturer” are Heather Ann Prentice, PhD, MPH; Dhiren S. Sheth, MD, FAAOS; Nithin C. Reddy, MD; Monti Khatod, MD, FAAOS; and Liz Paxton, PhD.
Rebecca Araujo is the managing editor of AAOS Now. She can be reached at raraujo@aaos.org.