A retrospective study presented during the AAOS 2024 Annual Meeting investigated whether there were any differences in postoperative outcomes and healthcare costs associated with total hip arthroplasty (THA) procedures performed on weekdays and weekends. The study was presented as a poster by Shawn Okpara, orthopaedic surgery resident at Baylor College of Medicine in Houston, Texas.
“The ‘weekend effect’ is the phenomenon that claims increased adverse outcomes for weekend procedures compared to weekday procedures. However, there is significant controversy regarding such disparities for elective orthopaedic surgeries,” the authors wrote in their study. Given the projected increases in demand for THA over the coming decades, “It is important to investigate a possible ‘weekend effect’ to optimize outcomes and cost effectiveness.”
The investigators utilized the Healthcare Cost and Utilization Project database, which includes hospital care data in the United States, to collect data on THAs performed between 2002 and 2020, including patient demographics, comorbidities, hospital length of stay (LOS), time from admission to procedure, discharge disposition, mortality, and postoperative outcomes. Data were compared between patients treated between Monday through Friday and those treated on Saturday to Sunday. For the statistical analysis, the researchers used independent sample t-tests to assess normally distributed data, and they used Wilcoxon rank-sum analysis for non-normally distributed data. To assess categorical variables, they used Fisher’s exact test or chi square with Kendall’s tau.
In total, data from 872,584 patients were analyzed, with the weekday group comprising 869,067 patients and the weekend group comprising 3,517. Weekend patients were more likely to be Black or Hispanic (P <0.001) and were also more likely to have medicaid insurance (>P <0.001). the average age of patients treated on weekends versus weekdays was older (67 years versus 64.5 years, respectively;>P <0.001). patients treated on weekends were more likely to have concurrent comorbidities than patients treated on weekdays. pneumonia, arrhythmia, heart failure and myocardial infarction, stroke and sequelae, venous thromboembolism (including deep vein thrombosis), hemorrhagic anemia, and acute or chronic kidney disease were all significantly more common concurrent diagnoses in the weekend group.
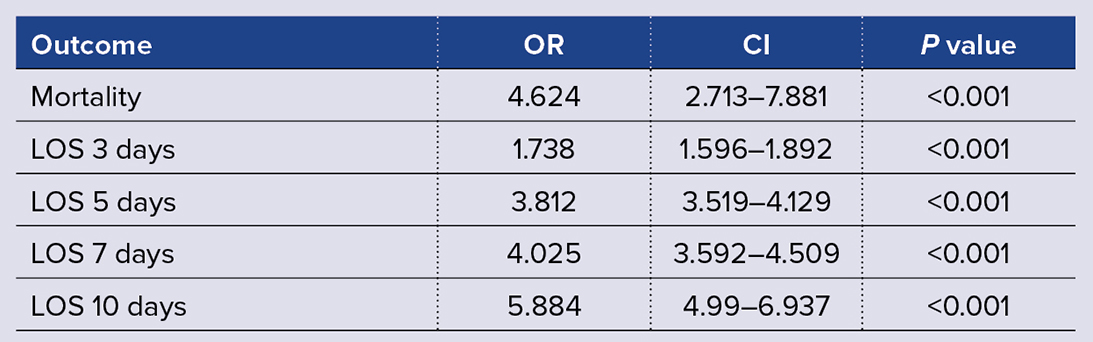
Weekday patients had a significantly shorter time from admission to procedure, at an average of 1.32 hours versus 14.04 hours in the weekend group (P <0.001). los was also greater for the weekend cohort, who averaged 4.32 days compared with 3.044 days (>P <0.001). mortality rates were 0.43 percent in the weekend tha group and 0.09 percent in the weekday tha group (>P <0.001). weekend thas were associated with significantly greater odds of an los of 3 or more days, along with greater odds of mortality (table 1).
Surgeries performed over the weekend were more likely to lead to an adverse discharge than weekday procedures (39.31 percent versus 28.39 percent; P <0.001). rates of home discharge with care after surgery were similar between groups. regarding costs, total charges were higher in the weekend group, at an average of $59,303.897 (± $40,399.768) compared with $50,701.736 (± $30,672.913) (>P <0.001).
In summary, the authors wrote, “We found that THAs performed on weekends were associated with significantly increased LOS, total charges, admission-to-procedure time, and mortality compared to those on weekdays.” They reported that these findings from centers across the United States are in line with other hospital-specific studies. The study is limited by the use of a database, which does not provide insights into factors such as hospital staffing, surgeon experience, availability of implants and equipment, and availability of care teams for the weekend versus weekday groups—all factors that may contribute to differences in outcomes based on the day of surgery.
Based on these results, the authors recommended efforts to optimize preoperative planning as well as identification of risk factors that would help identify patients at risk of increased LOS and poor outcomes with weekend procedures. They added, “Our findings suggest that the development of nationwide programs to standardize care, discharge planning, and weekend case management for THA patients can potentially help reduce healthcare costs, improve operative outcomes, and reduce the discrepancy between weekend and weekday surgeries.”
Poster P202 will be available during Practice Management/Rehabilitation II, Wednesday and Thursday in OrthoLive, located in West Hall.
Dr. Okpara’s coauthors of “Weekend versus Weekday Procedures for Total Hip Arthroplasties” are David A. Momtaz; Tucker J. Cushing, MD; Abdullah Ghali, MD; Travis Mark Kotzur, PhD; Parker Mitchell, MD; Albert Han; Adam Dylan Pearl; Varun Bora, MD; Ali Seifi, MD; and Khaled J. Saleh, MD.
Rebecca Araujo is the managing editor of AAOS Now. She can be reached at raraujo@aaos.org.