In older patients with complex proximal humeral fractures, reverse shoulder arthroplasty (RSA) provided a limited benefit compared with nonoperative treatment, according to results from a randomized clinical trial. The findings were presented as an ePoster at the AAOS 2024 Annual Meeting.
“There is increasing research focused on surgical techniques for proximal humeral fractures. However, there is limited research exploring the benefits of those surgical procedures over nonoperative treatment,” study coauthor Joan Miquel, orthopaedic surgeon at the Parc Taulí Hospital Universitari in Sabadell, Spain, told AAOS Now Daily Edition. Comparing these two management approaches “is helpful for patients’ decision-making process, as surgeons tend to overestimate the [benefits of] operative treatment,” he added.
The multicenter trial enrolled 81 patients aged 70 years or older who sustained an acute complex proximal humeral fracture (3 or 4 parts) and who had no previous condition or surgery on the affected shoulder. Patients with severely displaced fractures were excluded. Severely displaced fractures were those with no contact between fragments of the humeral head and diaphysis. Sixty-six patients completed the 1-year follow-up evaluation. Patients were randomized to RSA through the deltopectoral approach with tuberosities reattachment or nonoperative treatment, which consisted of the use of a sling for 3 weeks. Both treatment groups underwent a rehabilitative protocol following treatment. The Constant-Murley score at 1-year follow-up was used to assess functional outcomes. Secondary outcomes included complications and reinterventions.
Among the 66 patients available for 1-year follow-up, there were no significant differences in outcomes between groups according to patient age (P = 0.43), gender (P = 0.72), or Neer’s fracture classification (P = 0.06). Overall, Dr. Miquel reported, “Participants presenting with a displaced proximal humeral fracture and allocated to the surgical group obtained better outcomes than those assigned to nonoperative treatment. However, the benefit was unlikely to be perceived by participants,” he noted, as the difference in Constant-Murley scores was less than 9 points out of 100. Additionally, “The risk of complications was higher in the surgical group,” he said.
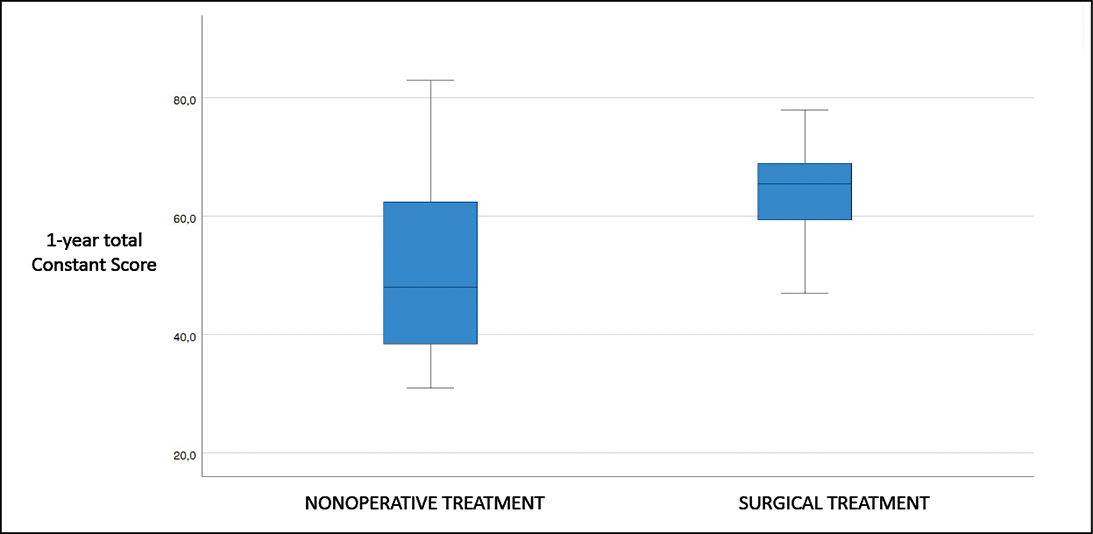
The mean Constant-Murley scores in the operative and nonoperative groups were 61.24 (standard deviation, 13.33) and 52.44 (standard deviation, 16.22) (Fig. 1). The 95 percent confidence interval for the difference between groups was 1.57 to 16.11.
No major complications or reinterventions were observed in the nonoperative group. Two patients who underwent surgery (6.5 percent) had major complications: one case each of periprosthetic joint infection (which required secondary surgery) and axillar nerve palsy.
Regarding limitations, given that the study did not include patients with severely displaced proximal humeral fractures, the present study does not provide helpful information for such cases, Dr. Miquel said. He also noted that the use of other patient-reported outcome measures beyond the Constant-Murley score “may help to interpret the benefits [of each intervention] from the patients’ perspective.”
Based on these findings, Dr. Miquel said, “There is a necessity to explore the benefits of surgical treatment by the use of RSA over nonoperative treatment for patients sustaining a proximal humeral fracture based on the extent of displacement. The publication of subsequent randomized trials about this specific question may be helpful for patients’ decision making.”
Poster e412 is available to view via the AAOS Annual Meeting Mobile App or online at aaos.org/ameducation.
Dr. Miquel’s coauthors of “Reverse or Nothing for Complex Proximal Humeral Fractures: Results of a Multicentric, Prospective Randomized Control Trial,” are Elisa Cassart, MD, PhD; Fernando Santana Perez, MD; Raquel Martinez Torregrosa; Laura Valls Bartrolí; Monica Salomo Domenech; and Carlos Torrens, MD.
Rebecca Araujo is the managing editor of AAOS Now. She can be reached at raraujo@aaos.org.