A study presented at the 2024 Annual Meeting investigated the impact of postoperative NSAIDs on clinical outcomes, return to activities, and rates of revision surgery in patients undergoing arthroscopic glenoid labral repair for glenohumeral instability.
“Arthroscopic labral repair has become a routine and effective outpatient procedure for active patients with glenohumeral instability,” Zachary Li, BA, presenting author and medical student at Tufts University School of Medicine, told AAOS Now Daily Edition. “NSAIDs are commonly utilized in multimodal postoperative pain-control protocols following orthopaedic surgery, but some surgeons remain hesitant, as these agents may theoretically interfere with the cyclooxygenase-mediated inflammatory cascade and potentially impede healing. At the same time, the opioid epidemic remains a significant problem in the United States, with drug overdose deaths continuing to rise.”
Mr. Li, who recently completed a clinical research fellowship in the Division of Sports Medicine in the Department of Orthopedic Surgery at NYU Langone Health in New York City, cited a prior randomized, controlled trial conducted at the institution as a catalyst for the present study. The study, published in December 2020 in Arthroscopy, Sports Medicine, and Rehabilitation, found significantly lower opioid use in the immediate postoperative period without a significant difference in pain levels or patient satisfaction between the use of NSAIDs or standard oral opioids in patients undergoing arthroscopic shoulder capsulolabral repair for recurrent anterior shoulder instability. Kirk Campbell, MD, FAAOS, associate professor in the Department of Orthopedic Surgery at NYU Langone Health, was the senior author of both the prior study as well as the present study. Dr. Campbell commented, “Given that we previously observed similar efficacy in pain control and decreased opioid usage when prescribing NSAIDs following labral repair, we now aimed to examine whether there would be differences in patient-reported outcomes, RTS/RTW [return to sport/work], and recurrent instability at a minimum 2-year follow-up following all labral repairs when comparing patients who received NSAIDs as part of their postoperative pain-management regimen with those who did not.”
The study, conducted at NYU Langone Health, involved a retrospective review of patients aged 18 to 55 years who underwent primary arthroscopic labral repair. Patients with concomitant rotator cuff repair and those lacking a minimum 2-year postoperative follow-up were excluded. Patients who received postoperative NSAIDs and those who received opioids alone were propensity matched in a 1:1 ratio based on age, sex, BMI, and number of anchors.
Patient-reported outcomes (PROs) were evaluated via the visual analog scale (VAS) for pain, the American Shoulder and Elbow Surgeons (ASES) score, the Simple Shoulder Test (SST), the Single Assessment Numeric Evaluation (SANE), and satisfaction. Additionally, data on preinjury sport participation and work activity, along with their subsequent resumption, were documented. The study also recorded complications and revision procedures occurring within the 2-year period following the index surgery.
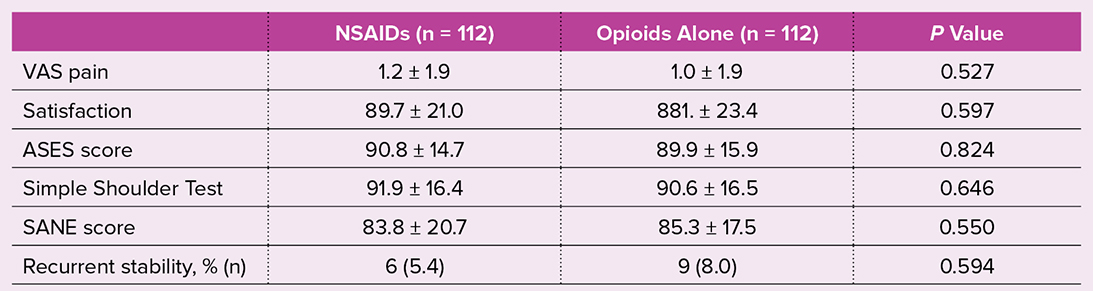
Among the 269 patients who completed all PRO measurements, 224 were successfully matched (mean age: 32.2 ± 9.8 years; BMI: 26.0 ± 4.5; 80.8 percent male). As shown in Table 1, functional and recovery outcomes were similar between groups. VAS pain scores were not significantly different between patients who received NSAIDs and those who did not (1.2 and 1.0, respectively). Additionally, patients receiving NSAIDs showed no significant differences in ASES (90.8 versus 89.9), SST (91.9 versus 90.6), or SANE (83.8 versus 85.3) scores compared with non-NSAID recipients.
The RTS rate was 83.5 percent in the NSAIDs group and 77.8 percent in the non-NSAIDs group (P = 0.318), with similar rates of return to preinjury sport levels (59.3 percent versus 61.6 percent, respectively; P = 0.177). The majority of patients in both groups resumed their prior work (93.3 percent versus 95.3 percent, respectively; P = 0.617).
Revision surgery rates (2.7 percent versus 0.9 percent, P = 0.622) and the incidence of recurrent instability (5.4 percent versus 8.0 percent, P = 0.594) were comparable between the NSAID and non-NSAID groups. Multivariable regression analysis revealed no significant association between postoperative NSAIDs and subsequent revision (odds ratio [OR]: 1.265, P = 0.779), RTS (OR: 1.621, P = 0.173), or RTW (OR: 1.158, P = 0.793).
“An interesting aspect of the results was that there was also no significant difference in the time taken to return to sport or work,” Mr. Li said regarding the results. “One might hypothesize that if NSAIDs were not controlling pain effectively or impeding healing, there may be an increased delay to return to activities. This was not shown in our results.” Therefore, according to Mr. Li, these results “should provide additional assurance to surgeons in prescribing NSAIDs postoperatively for labral repair.”
Paper 170 will be presented during Sports Medicine II, Wednesday at 11 a.m. in West, Room 2001.
Mr. Li’s coauthors of “The Effect of Postoperative Non-Steroidal Anti-Inflammatory Medications on Arthroscopic Glenoid Labral Repair: Clinical Outcomes and Return to Sport at Minimum 2-Year Follow Up” are Sharif Garra, MD; Nathan A. Huebschmann, BA; Jordan Eskenazi, BS; Jairo Triana, BS; Edward S. Mojica, MD; Michael J. Alaia, MD, FAAOS; Eric J. Strauss, MD, FAAOS; Laith M. Jazrawi, MD, FAAOS; and Kirk A. Campbell, MD, FAAOS.
Cailin Conner is the associate editor of AAOS Now. She can be reached at cconner@aaos.org.
References
- Thompson KA, Klein D, Alaia MJ, ET AL: Opioid use is reduced in patients treated with NSAIDs after arthroscopic Bankart repair: a randomized controlled study. Arthrosc Sports Med Rehabil 2020;3(1):e15-e22.