A study presented at the AAOS 2024 Annual Meeting investigated the benefit of robotic assistance as measured by risk of revision 2 years after total knee arthroplasty (TKA) with cementless fixation in patients aged 65 years or older, using data from the American Joint Replacement Registry (AJRR). The findings were presented by Lucas Nikkel, MD, assistant professor of orthopaedic surgery at Johns Hopkins University.
According to Dr. Nikkel, “Multiple studies continue to note dissatisfaction among some percentage of patients after knee replacement operations, and at a much higher rate than following hip replacement.” He noted an “explosion of interest” in the use of robotic technology and cementless components for this procedure. However, “Many of the studies on robotic assistance have been small or authors have had significant financial conflicts, and marketing has amplified the idea and implication that precise and accurate bone cuts make for a better knee replacement,” he told AAOS Now Daily Edition.
The investigators assessed data from 9,220 cases of patients aged 65 or older who underwent primary TKA for osteoarthritis with cementless femoral and tibial components between January 2017 and March 2020. The study utilized Medicare claims data to assess 2-year outcomes. Robotic assistance was used in 44.8 percent of cases.
“The major findings of the study were that there was no difference in risk of revision 2 years after the knee replacement with or without use of robotic assistance when using cementless knee replacement implants,” Dr. Nikkel summarized. The rate of all-cause 2-year revision was 1.16 percent with robotic TKA versus 1.3 percent with conventional TKA (P = 0.6), with no statistical difference in a mixed-effects logistic regression analysis (P = 0.4).
Though he noted surprise at this outcome, Dr. Nikkel acknowledged, “This finding is in line with data we previously published looking at the effect of robotic assistance on revision risk 2 years after knee replacement surgery among all types of implants [Kirchner et al., Clinical Orthopaedics and Related Research, November 2023] and in line with findings from the Australian Orthopaedic Association National Joint Replacement Registry, which found similar risk of revision with and without robotic assistance, although they did not stratify by cemented or cementless fixation methods.”
Dr. Nikkel also said, given that “cementless implants are often used in younger patients with better bone quality, we would have expected a slightly higher failure rate of cementless implants in older patients and therefore a greater ability to detect or isolate the benefit of robotic assistance.”
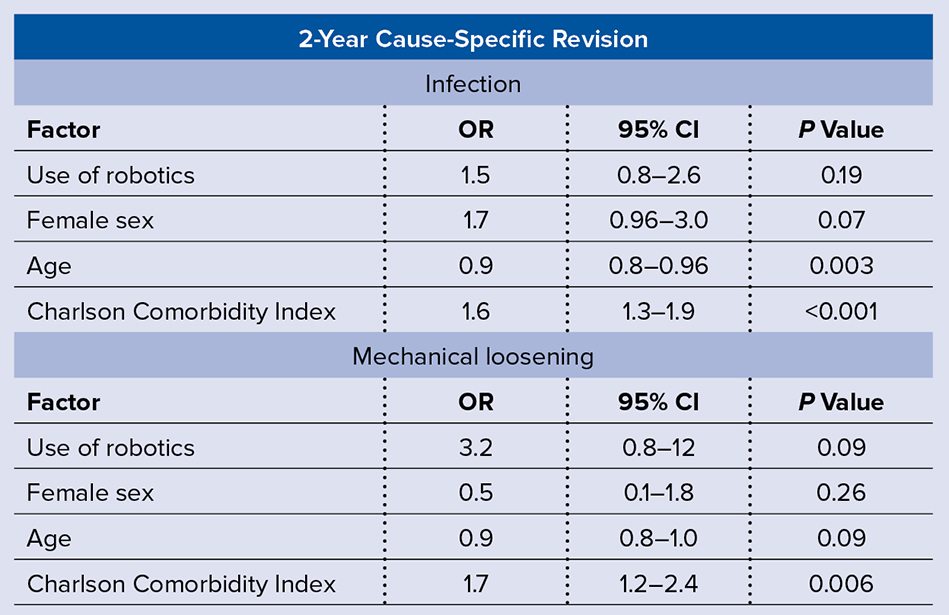
Univariate analysis found that robotic-assisted TKA was associated with a significantly higher risk of revision for infection (P = 0.026) and mechanical loosening (P = 0.03); however, this relationship was attenuated after the researchers controlled for age, sex, and Charlson Comorbidity Index.
The study had several limitations, such as being limited to older patients and only using revision as an endpoint. A small sample size was another limiting factor. “As robotics and cementless implants are both emerging technologies, there were insufficient numbers of patients in the study to determine if specific reasons for revision varied between patients undergoing robotic-assisted and conventional knee replacement,” Dr. Nikkel commented. He also noted insufficient data capture to separately evaluate patient-reported outcome measures at the 2-year follow-up timeframe, which could miss any differences in long-term outcomes.
For future studies, Dr. Nikkel advised looking at other outcomes apart from revision and loosening to gauge the benefit of robotic assistance. “Revision knee replacement surgery is not the only important metric in patient outcome after knee replacement surgery; range of motion, sensation of stability, forgotten joint score, and rate of recovery are all important areas of future study, and robotic assistance has the potential to improve outcomes in these areas,” he said.
Paper 309 will be presented during Adult Reconstruction Knee IV, 11 a.m. on Thursday in West, Room 2001.
Dr. Nikkel’s coauthors of “Effect of Robotic Assistance on Early Revisions and Aseptic Loosening in Cementless Total Knee Arthroplasty: An Analysis of the American Joint Replacement Registry” are Gregory J. Kirchner, MD, MPH; Jeffrey B. Stambough, MD; Emily Jimenez, MPH; and Kyle Mullen, MPH.
Rebecca Araujo is the managing editor of AAOS Now. She can be reached at raraujo@aaos.org.
Reference
- Kirchner GJ, Stambough JB, Jimenez E, et al: Robotic-assisted TKA is not associated with decreased odds of early revision: an analysis of the American Joint Replacement Registry. Clin Orthop Relat Res 2023;482(2):303-10.