For patients with presumed atraumatic rotator cuff tears (RCTs), it is common for insurance companies to mandate 6 weeks of conservative physical therapy (PT) prior to approval for order of MRIs.
According to Caroline Gutowski, BS, medical student at Cooper Medical School of Rowan University and presenting author of a study at the AAOS 2024 Annual Meeting, “In practice, the physicians at our institution have faced pushback from insurance companies for MRI orders upon initial consultation. In these circumstances, despite a specialist’s strong clinical suspicion for an RCT (e.g., significant weakness on exam, pain for extended periods of time not improving with rest, NSAIDS, etc.) and recommendation for timely imaging, many health insurance payers mandate 6 weeks of formal PT prior to authorizing imaging orders.”
In their study, Ms. Gutowski and colleagues sought to quantify the number of positive full- and partial-thickness tear findings via MRI compared with clinical examination at initial consultation, “to provide evidence-based support for an orthopaedic specialist’s indication for timely imaging,” she told AAOS Now Daily Edition.
This retrospective review included 403 patients aged 18 years or older who had an MRI ordered at their first visit with an orthopaedic shoulder specialist. The primary outcome was the presence or absence of an RCT, and the secondary outcome was subsequent surgery.
The researchers also conducted subgroup analyses of tears based on insurance status, previous PT/steroid injection of the ipsilateral shoulder, and ordering physician.
“We wanted to see if a documented history of PT and/or injection of the ipsilateral shoulder would impact a clinician’s suspicion for a tear; thus, we further stratified patients by whether they had a documented history of either,” Ms. Gutowski explained. They also assessed the average costs of 6 weeks of PT versus the cost of immediate MRI.
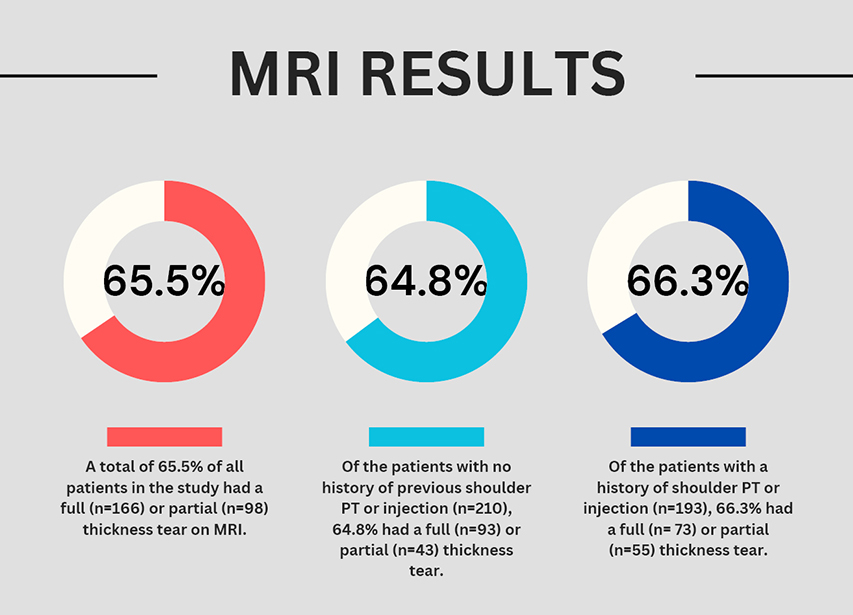
Fig. 1 demonstrates rates of confirmed RCTs via MRI. Overall, MRI review found that 41.2 percent of patients presented with a full-thickness tear, 24.3 percent had a partial-thickness tear, and 34.5 percent had no tear. Of the patients with a full-thickness tear, 57.8 percent proceeded to surgery. In the subgroup analysis of 210 patients with a documented history of PT and/or injection, 64.8 percent had positive MRI findings for either a full- or partial-thickness tear (n = 93 and 43, respectively). Among the 193 patients with a documented history of conservative therapy, 66.3 percent were found to have a full- or partial-thickness tear on MRI (n = 73 and 5, respectively).
“The positive yield of MRI imaging remained at 64.8 percent in the absence of a documented history of conversative treatment, which, while not exactly unexpected, was pleasantly validating. It further supports a specialist’s clinical suspicion of tear on history and physical exam in office,” Ms. Gutowski noted. “We were, however, surprised that only 57.8 percent of patients went on to surgery.”
According to Ms. Gutowski, “This study demonstrated that orthopaedic specialists have a high yield rate when identifying rotator cuff tears by MRI based on history and physical exam upon initial consultation. Six weeks of mandated PT by insurance companies delays diagnoses and thus may delay treatment interventions.”
Regarding costs, at the institution assessed, the cost of an upper-extremity MRI without contrast averaged $2,268, whereas two sessions of PT per week for 6 weeks totaled $2,328 ($194 per session). “Pre-MRI PT when early imaging is warranted only adds additional healthcare costs,” Ms. Gutowski commented.
Importantly, she added, “The goal of this study is not to discredit the value of PT, but instead to emphasize that the decision of PT versus early MRI diagnosis might be better made by a specialized clinician rather than insurance companies.”
Ms. Gutowski acknowledged several limitations to this study, including its retrospective design. Additionally, “The specific length or type of previous PT patients underwent was not assessed, as it was beyond the scope of this paper. Clinical outcomes for patients were also not included in the study and thus limits comparison,” she acknowledged.
Based on these findings, Ms. Gutowski called for future studies “comparing MRI results and clinical outcomes between patients who received preauthorization for MRI and those who underwent the 6 weeks of conservative therapy before MRI. These studies will better clarify the impact of potential delays in diagnoses and thus surgical intervention.”
Paper 343 will be presented during Shoulder and Elbow III, 1:30 p.m. on Thursday in South, Esplanade Ballroom 155.
Ms. Gutowski’s coauthors of “Accuracy of Clinical Suspicion for Rotator Cuff Tear by Orthopaedic Surgeons when MRI Ordered on Initial Visit: Should Physical Therapy be Mandated by Insurance?” are Nicholas Pohl, BS; Matthew Stern, BS; Pietro Gentile, BS; Christopher Rivera-Pintado, MD; Parker Johnsen, MD; and Catherine Fedorka, MD.
Rebecca Araujo is the managing editor of AAOS Now. She can be reached at raraujo@aaos.org.