WellStar Health System, the largest health system in Georgia, comprised of 11 hospitals and 225 medical office locations, is focused on improving quality and access to health care. It operates outpatient centers, health parks, a pediatric center, nursing centers, hospice, and a home care agency.
As the system expands through both hospital acquisition and network partnerships, the creation of a centralized public reporting process became a priority. Restructuring its reporting approach addressed multiple needs, including more unified and integrated data collection across all public reporting efforts and a more efficient way to manage the complex needs of multiple registries. WellStar currently participates in many multispecialty-driven registries, including the American Joint Replacement Registry (AJRR).*
The new systemwide reporting process was specifically designed to help take fragmentation out of healthcare delivery. Physicians and clinical staff now share broader data access and increased opportunities to consult with colleagues across the healthcare system. This helps coordinate all the elements of patient care and provides a more comprehensive, less fragmented view of clinical activities and outcomes. Increasing access to the system’s integrated data also allows WellStar to better understand and address the aggregate needs of its patients in the greater Atlanta community.
Data activity areas
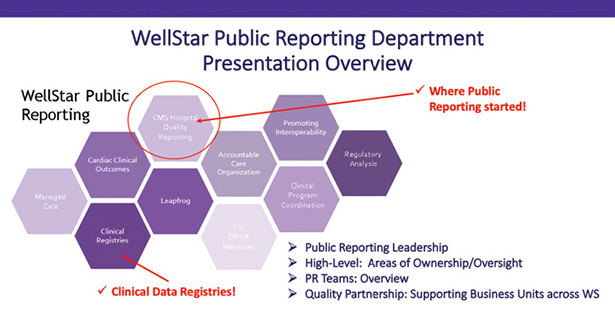
Now, the public reporting department at WellStar is divided into four general data activity areas, creating a focused home for all public reporting efforts (Fig. 1):
- mandatory hospital and ambulatory performance data driven by the Centers for Medicare & Medicaid Services (CMS) and The Joint Commission (TJC)
- quality program registries (like AJRR)
- cardiac clinical outcomes data
- privately managed care quality surveys and accountable care organization data
Dori Ledford, MHA, MBA, BS-IT, director of public reporting at WellStar, with a management staff of four, created a new department structure that originally started as a support area for addressing CMS Hospital Reporting. The restructuring was to keep pace with an increasing variety of public reporting needs (Fig. 1) and to accommodate the internal demand for registry clinical/surgical patient data. The data, for example AJRR, are used exclusively in WellStar quality control and improvement efforts. They also created a dynamic internal public reporting communication platform to support these same efforts (Fig. 2).
Where we are
Currently, five WellStar hospitals with a large volume of “non-[WellStar] employed” physicians collectively perform 200 to 230 arthroplasties per month. Like many healthcare systems involved with AJRR, not all WellStar hospitals began registry participation at the same time.
A phased system approach is often required due to one or more of the following factors: (1) desire for one hospital to establish a successful registry process as a model for the rest of the system; (2) operational issues, like disparate electronic health records (EHRs) and other conflicting data sources, that need to be resolved; and (3) information technology (IT), full-time employees (FTEs), and other resource constraints.
Pain points, lessons learned, and AJRR’s new home
WellStar has been an AJRR participant since 2015 and has submitted more than 4,210 hip (44.78 percent) and knee (55.22 percent) arthroplasty procedures to the registry as of March. Mrs. Ledford described her team’s past and present challenges in optimizing registry participation to help achieve her organization’s goals: “While some of the issues can be daunting at times, the collaborative partnership between AJRR, WellStar’s data registry coordinators, and the surgeons we support is already promising to have far-reaching effects when it comes to the collection and analysis of data on patients’ experiences and outcomes.”
WellStar’s primary “pain points,” mitigated through recent efforts, continue to include:
- Non-WellStar–employed physicians are engaged as “affiliate providers” where the independent reporting systems they use (outside the system) may not be compatible with WellStar.
- Within the system, disparate data sources remain due to WellStar’s rapid growth; there often are disparate EHR software/vendors and patient questionnaire vendors within the system and in its network of partners.
- Finding the appropriate data from patient-reported outcome (PRO) questionnaires and verifying the data are within the reportable date range.
- Because WellStar has multiple users and registries, a wish list item involves finding, sharing, and connecting with other registry innovators; finding the right connections, at the right time, remains a challenge.
- WellStar health technology is at a crossroad between an internal EHR build (Epic) and operational consolidation.
WellStar success to date and lessons learned
Some WellStar Registry “lessons learned” include the importance of:
- strong surgical champions who can keep engagement and momentum going among clinical peer stakeholders
- establishing a systemwide committee structure that connects surgeon and clinician leadership in real time, thereby enabling effective public reporting and registry decision support
- diversified resource teams, including engaged clinicians, collaborative IT (layout data/workflow validation), and business partners
- standardizing wherever possible, including workflow to data element mapping (widespread use of templates and discrete data fields)
- hiring lead FTEs with high abstract reasoning skills, medical/technical acumen, creative problem-solving, and self-starter qualities
- communication at all levels is an important key to public reporting success, including the registries component
Where WellStar’s AJRR development is going within its public reporting home
WellStar’s interim surgical champion for AJRR and Vice Service Line Leader W. A. (Tony) Griffith, MD, FACS, said, “AJRR contributes to WellStar’s ability to deliver consistent, evidence-based, high-quality orthopaedic care across the board. Reviewing our registry data helps us proactively identify what works or doesn’t. Our clinical team(s) can then work together to resolve issues and improve patient care more quickly. The term high reliability can be a cliché, but at WellStar, there is a genuine desire to have a continuous improvement process in place.”
Optimizing WellStar’s AJRR performance going forward will require:
- obtaining data share agreements with AAOS Registry Program authorized vendor partners to help reduce some of the burden of extracting patient-reported data
- maximizing AJRR’s Registry-
Insights® platform capabilities including PRO measures, which was launched at WellStar’s Kennestone Hospital earlier this year - continuing use of AJRR to help support TJC advanced total hip and total knee replacement certification for WellStar’s Kennestone Hospital; AJRR is the sole registry pathway, recognized by TJC, for this certification
- working with WellStar IT to complete a standardized “Epic Template Build” for AJRR/Op Note specifications pertaining to AJRR data element requirements; the Op Note is Epic’s surgical narrative application/module
- limiting data backlog to ensure efficient and accurate crossover to AJRR
Mrs. Ledford concluded, “AJRR’s data can facilitate public reporting, retrospective and prospective exploration, professional development, and service improvement. Most importantly, we will look to this data to reveal variations in practices, processes, and outcomes and identify targets for improvement.”
Access other peer-to-peer registry case studies and presentations through Unet
If you found value in WellStar’s “lessons learned,” as a subscriber you can activate communication with other registry subscribers in the AAOS User Group Network (Unet). To participate, create a Unet Forum account at www.ajrr.net/forum.
Karen Metropulos, MBA, is a content writer at AAOS. She can be reached at metropulos@aaos.org.
*WellStar participates in AJRR and a variety of other independent registries such as Cardiac Arrest Registry to Enhance Survival, Setting Scoliosis Straight Surgeon Performance Program, NeuroVascular Quality Initiative, and the Quality Outcomes Database.
