In the knee, articular cartilage defects are common. An incidence of up to 60 percent, of which 5 percent to 10 percent are full-thickness lesions, has been reported after arthroscopic evaluations. Although many findings are incidental, others can be symptomatic and progressive, resulting in pain and dysfunction. Due to the inability of articular cartilage to heal, many strategies have been developed for cartilage restoration. Despite advancements in surgical strategies, ongoing limitations in the ability to restore true hyaline cartilage continues to pose a significant challenge.
Treatment strategies for symptomatic cartilage defects are typically grouped into reparative or restorative. Reparative options include direct fixation of large osteochondral lesions and marrow stimulation-type procedures to promote a healing response. Restorative techniques can be further classified into surface-type strategies, such as allogenic or autogenic compounds and cellular matrices applied on top of the subchondral plate, or composite options containing both hyaline cartilage and bone to address deep lesions. Specifically, this includes osteochondral autograft and allograft transplantation.
Determining the most appropriate strategy depends on lesion characteristics, pathogenesis, and patient factors. There is no “one size fits all” strategy when it comes to cartilage restoration. Success depends not only on the appropriate application of the available options but also on patient selection. Acknowledging that not all “found” cartilage lesions require treatment is paramount. Arthroscopic and MRI findings must be correlated with a thorough history, patient symptoms, and physical examination to be deemed symptomatic and appropriate for treatment. Preoperative workup necessitates the assessment of lower-extremity alignment, meniscal status, and ligamentous stability. Associated correctable pathology should be identified and addressed with judicious use of osteotomies to improve joint mechanics. The most challenging aspect, however, is preoperative surgical planning based on patient and lesion characteristics.


Osteochondral autograft transplantation
Osteochondral autograft transplantation is typically reserved for restoration of small defects. This technique involves harvesting donor osteochondral plugs from low load zones about the knee and transferring them to the recipient site. Advantages of autografts include the ability to be performed as a single-stage procedure, low cost, and avoidance of disease transmission. Major disadvantages of this technique include availability of transferable nonessential cartilage, as well as donor site morbidity. This imparts a limitation on the size of the treatable lesion. Typically, autograft transfer is not recommended for cartilage lesions greater than 2 cm2 in size, and plug diameter is generally kept to around 1 cm to minimize donor site morbidity.
Autograft transfers have been proven to be durable with good results even in high-demand patients. Although direct comparison of autograft to allograft procedures is difficult based on inherent discrepancies in lesion size, autograft transfers have demonstrated improved clinical outcomes compared to patients treated with microfracture with up to 10 to 15 years of follow-up.
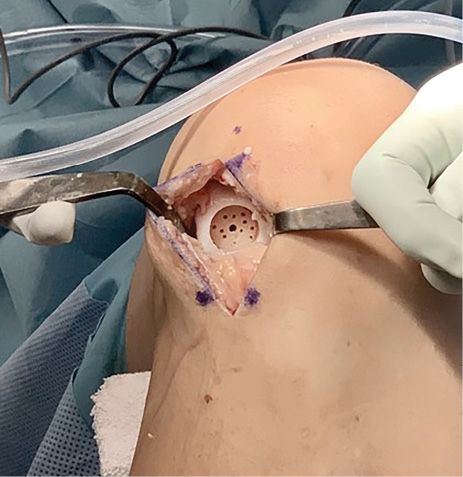
Osteochondral allograft transplantation
Osteochondral allograft transplantation (OCA) is the preferred technique to address medium to large lesions involving subchondral bone, as well as revisions of marrow stimulation or surface-type treatments. An advantage of this technique is the ability to address larger defects with immediately stable hyaline cartilage without donor site morbidity. However, unlike autograft, a rejection response may be mounted against the marrow elements in the transplanted bone. The downsides of this technique are graft availability, cost (with grafts approaching upward of $10,000), and the risk of disease transmission. Chondrocyte viability decreases after harvest, and a window of 28 days from graft harvest to implantation is currently recommended. Fresh osteochondral allografts are typically stored at a tissue bank until microbiologic and serologic testing is completed, significantly decreasing the window available for implantation. New preservation techniques such as the Missouri Osteochondral Allograft Preservation System may lengthen the time window, subsequently increasing graft availability. The protocol has recently demonstrated the ability to maintain adequate allograft chondrocyte viability for more than 56 days.
Limited tissue availability has driven current investigations to examine utilization of available tissue and the viability of nonorthotopic grafts (e.g., using a lateral femoral condyle graft for a medial femoral condyle defect). Recent studies suggest that nonorthotopic grafts may restore native cartilage anatomy without compromising graft survival. Nonorthotopic graft use effectively increases the supply and utilization of available donor cartilage, thus reducing the wait time for those in need.
The versatility of allograft use has also been expanded to the patellofemoral compartment—an area historically avoided. Several recent studies have demonstrated the benefits of using osteochondral allografts to address complicated isolated and bipolar lesions in the patellofemoral compartment. Although long-term data are limited, five- and 10-year graft survival rates of 87 percent and 77 percent, respectively, have been demonstrated, along with significant improvements in patient-reported outcomes (PROs).
Conclusion
Overall, OCA has demonstrated excellent long-term outcomes, with consistent improvements in PRO measures, as well as reliable return to prior levels of activity. Graft survivorship has been demonstrated to be approximately 90 percent at five to 10 years, with return to high levels of physical activity in approximately 80 percent of patients. The preferred technique is to use autograft when lesion size is appropriate and allograft for addressing medium to large defects and revision situations. Alignment, ligamentous instability, and meniscal deficiency are typically addressed concomitantly to maximize graft survivorship.
Mikhail Alexeev, MD, is a member of the Department of Orthopaedic Surgery at WellStar Atlanta Medical Center.
James S. Kercher, MD, is a member of Peachtree Orthopedics in Atlanta, as well as the founder of the Atlanta Cartilage Restoration Center.
References
- Cavendish PA, Everhart JS, Peters NJ, et al: Osteochondral allograft transplantation for knee cartilage and osteochondral defects: a review of indications, technique, rehabilitation, and outcomes. JBJS Rev 2019;7:e7.
- Chahla J, Sweet MC, Okoroha KR, et al: Osteochondral allograft transplantation in the patellofemoral joint: a systematic review. Am J Sports Med 2018:363546518814236.
- Hjelle K, Solheim E, Strand T, et al: Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy 2002;18:730-4.
- Mirzayan R, Charles MD, Batech M, et al: Bipolar osteochondral allograft transplantation of the patella and trochlea. Cartilage 2018:1947603518796124.
- Mologne TS, Cory E, Hansen BC, et al: Osteochondral allograft transplant to the medial femoral condyle using a medial or lateral femoral condyle allograft: is there a difference in graft sources? Am J Sports Med 2014;42:2205-13.
- Richter DL, Tanksley JA, Miller MD: Osteochondral autograft transplantation: a review of the surgical technique and outcomes. Sports Med Arthrosc Rev 2016;24:74-8.
- Solheim E, Hegna J, Strand T, et al: Randomized study of long-term (15–17 years) outcome after microfracture versus mosaicplasty in knee articular cartilage defects. Am J Sports Med 2018;46:826-31.
- Stoker AM, Stannard JP, Kuroki K, et al: Validation of the Missouri Osteochondral Allograft Preservation System for the maintenance of osteochondral allograft quality during prolonged storage. Am J Sports Med 2018;46:58-65.
- Wang D, Jones KJ, Eliasberg CD, et al: Condyle-specific matching does not improve midterm clinical outcomes of osteochondral allograft transplantation in the knee. J Bone Joint Surg Am 2017;99:1614-20.
- Widuchowski W, Widuchowski J, Trzaska T: Articular cartilage defects: study of 25,124 knee arthroscopies. Knee 2007;14:177-82.