Posterior Sternoclavicular Joint Dislocation and Reconstruction
Background
Sternoclavicular joint dislocations are rare, accounting for only 1% to 3% of upper extremity injuries. Sternoclavicular joint dislocations may be life-threatening because of potential damage to vital structures, such as the trachea, esophagus, lungs, and nearby neurovascular structures. Prompt recognition and management of brachiocephalic vessel compression in patients with a posterior dislocation are crucial. Nonsurgical management involves closed reduction under general anesthesia; however, recurrence occurs in as many as 50% of patients. Irreducible dislocations may necessitate open reduction. Open reduction affords the best control for safe reduction in patients with a posterior dislocation given the risk of mediastinal structure injury. After reduction, ligament reconstruction provides stability without hardware complications.
Purpose
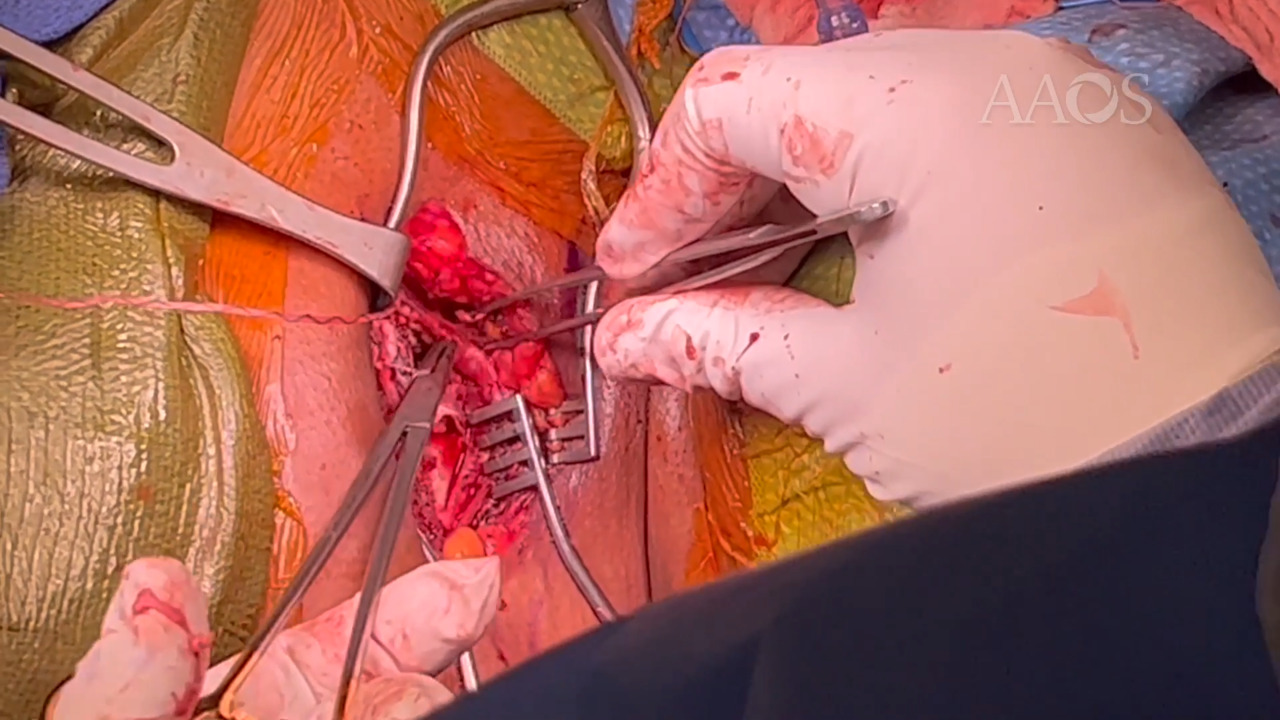
This video demonstrates the surgical technique for management of a posterior sternoclavicular joint dislocations via figure-of-8 reconstruction.
Methods
Evaluation, diagnosis, and management of posterior sternoclavicular joint dislocations are discussed. The case presentation of a 37-year-old man with a posterior sternoclavicular joint dislocation who was treated via figure-of-8 reconstruction is reviewed.
Results
The patient progressed through a standardized rehabilitation protocol. At 6 weeks postoperatively, the patient presented with considerable pain relief and a reduced sternoclavicular joint.
Conclusion
Posterior sternoclavicular joint dislocations may be life-threatening injuries and can cause compression or injury to the surrounding hilar structures. Reduction and surgical reconstruction of a posterior sternoclavicular joint injury can result in good radiographic and clinical outcomes.