Suture Bridge Fixation for Posterior Cruciate Ligament Tibial Avulsion Fracture in Children: A Report of Two Cases
Posterior cruciate ligament (PCL) tibial avulsion fracture is rare in the pediatric population. The mechanism of injury is a direct external force on the proximal anterior surface of the tibia or external forces, such as hyperextension, hyperflexion, or strong external rotation. In addition, the relative weakness of the physis and bone compared with the ligament in children more commonly results in osteochondral avulsion rather than ligamentous substance tear, which is observed in adults. Swelling of the knee joint often is difficult to identify in children with a PCL avulsion fracture, and range of motion often is not restricted. Especially in the acute phase, posterior instability often is unclear. If a patient who was hit in front of the lower leg shows the posterior drawer sign and sagging is positive, then PCL avulsion fracture or PCL substance injury should be suspected. Plain radiographs may be useful for detecting avulsed fragments if they are mostly osseous; however, osteochondral avulsions of the PCL in skeletally immature patients may be missed on plain radiographs if ossification is not complete and an abundance of cartilage is present. MRI is useful not only for diagnosing fractures but also for assessing PCL substance and comorbid injuries. Therefore, MRI should be considered.
In previous studies, bone fragment fixation methods have been classified as screw-based or anchor-based techniques. Disadvantages of the screw method include a risk of epiphyseal damage and destruction of the bone fragment. In addition, secondary surgery is necessary for implant removal. Conversely, the anchor method lacks fixation strength. The suture bridge technique is commonly used for arthroscopic rotator cuff repair and is relatively easy to perform. It is more effective for attaining high initial fixation strength. The literature on the management of PCL avulsion fractures via arthroscopic high-strength suture fixation is associated with good results. In addition, the anchor is driven into the bone, has a low profile, and does not require removal. With the suture bridge method, firm fixation of the bone fragment to the surface is possible and the risk of destruction of the bone fragment is decreased.
The first patient reviewed in this video is a 10-year-old girl who was hit in the front of her left lower leg while playing with a sled. The patient presented 2 weeks postinjury. Physical examination revealed swelling and subcutaneous bleeding in the front of the left lower leg. Patella ballottement, posterior sagging of the tibia, and the posterior drawer sign were observed. Plain radiographs of the left knee joint appeared normal. CT was performed because a PCL avulsion fracture was suspected based on the mechanism of injury and physical examination findings. CT scans showed a bone fragment approximately 2 × 15 mm in size, with 10 mm of displacement. MRIs showed a wavy PCL and bone bruise of the tibia. No meniscal tears were observed.
The second patient reviewed in this video is an 11-year-old girl who fell while playing tag and hit the front of her left lower leg. Although the pain improved, the patient could not flex her knee joint deeply. The patient presented 2 months postinjury. Posterior sagging of the left tibia was observed. In addition, the posterior drawer sign was positive. Plain radiographs demonstrated a PCL avulsion fracture of the left knee joint. MRIs showed a wavy PCL. No bone bruises of the femur and tibia or meniscal tears were observed.
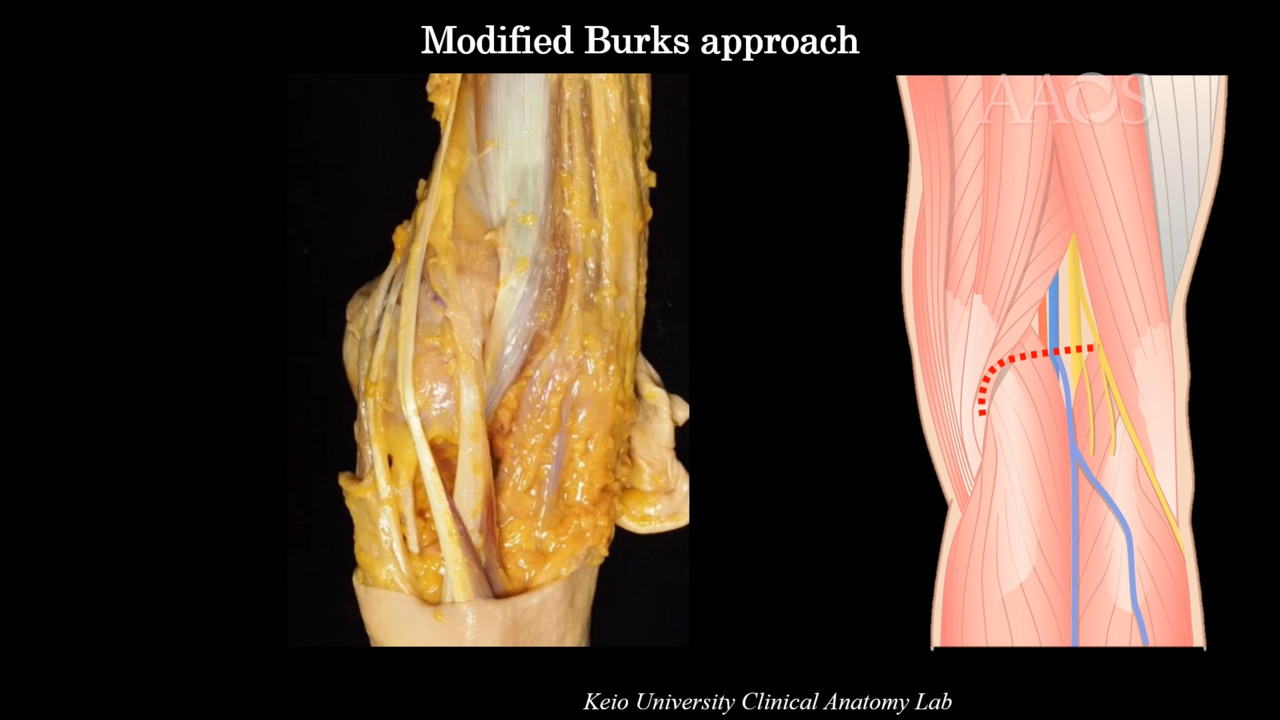
The patient was placed in the prone position on a standard surgical table. Surgical treatment was performed via a modified Burks approach. A skin incision was made by smoothly curving the lateral limb just below the crease of the hind knee to the vertical limb along the medial gastrocnemius muscle. A sterile tourniquet was applied to the upper thigh of the leg being managed. The skin incision was made as planned, and a blunt incision was made in the deep fascia along the medial head of the gastrocnemius muscle. The plane between the semimembranosus tendon and the medial head of the gastrocnemius muscle was developed, with the latter laterally protecting the gastrocnemius muscle. Incisions were made in the dorsal root of the oblique popliteal ligament and the joint capsule outside the dorsal root of the medial meniscus. The bone fragments and footprint were identified and dissected. The footprint and the bone fragment were dissected. Reduction was confirmed to be possible by threading the bone fragment and pulling it. Two soft anchors were placed on site. The suture was passed between the PCL and the bone fragment. The bone fragment was reduced via 90° flexion of the knee joint. The suture was pulled in, crossed, and anchored distally around the footprint. Finally, it was firmly fixed to the surface. Postoperatively, the patient wore a knee brace. Gentle range of motion training with physical therapist was allowed for 4 weeks, after which partial–weight bearing to pain tolerance was allowed. Return to sports activity was completed in stages based on recovery of muscle strength and stability of movement on the affected side.
The patient was able to walk independently 6 weeks postoperatively. Bone fusion was confirmed on CT scans obtained 8 weeks postoperatively. The patient returned to partial sports activity 12 weeks postoperatively. At 9 months postoperatively, the patient returned to full sports activity; range of motion was not restricted, and the patient was able to sit Japanese-style.
Pediatric PCL avulsion fractures are easily misdiagnosed on plain radiographs. A careful physical examination is necessary. If sagging or a posterior drawer sign is observed in a patient who sustained a strong hit from the front of the lower leg, MRI should be considered. In children, ossification is not complete, and an abundance of cartilage is present; therefore, screw fixation may easily destroy the bone fragment. The suture bridge method can be used to firmly fix the bone fragments. In addition, the risk of destroying the bone fragment is decreased, and secondary surgery for implant removal is not necessary.